Are quick learners at higher risk of post-traumatic stress? And more important, what can we do about it? Psychiatry experts came together in a recent national workshop to share ideas for more effective rehabilitation of the brain after trauma.
What do we do with a study showing that higher memory and vocabulary scores on cognitive tests seem to be associated with a higher risk of experiencing post-traumatic stress symptoms? Could research on this subgroup of quick learners who can't seem to lose the memory of a traumatic event provide insights that could lead to treatment possibilities? Discussions such as this were enlightening as psychiatry and neurology experts shared their findings at a recent national military medical research workshop.
Leading civilian and military researchers explored the state of knowledge related to brain dysfunction in an effort to increase progress in preventing and treating mental injury related to combat. The event was funded by the U.S. Army Medical Research and Materiel Command's Telemedicine and Advanced Technology Research Center.
Dr. Robert Ursano of the Uniformed Services University of the Health
Sciences presented the idea that the medical community must start treating post-traumatic stress more as we do a "common cold," thus reducing the stigma that prevents so many from seeking help. "It's a natural reaction," he said. "But we need to understand why it becomes chronic in some individuals." Ursano and co-investigator Dr. Murray Stein of the University of California, San Diego, were recently awarded the largest National Institute of Mental Health grant ever given for the study of suicide in the U.S. Army.
Ursano noted that neurobiological reactions to stress indicate a number of different research directions, and that defining post-traumatic stress disorder is the key to developing effective therapies. "For instance, if we look at PTSD as an inability to digest early stress symptoms and return to homeostatic balance, it may be best to study the startle reaction. If we think it's an altered set point, examining the cerebellum's role may be best. We could even think of PTSD as an autoimmune disorder in which the neurocognitive ability to identify with others, which is usually helpful in social interactions, leads to distress because of such intense identification with others' pain."
Dr. Roger Pitman of Harvard Medical School presented findings from the large-scale psychobiologic twin study he has been conducting for the past 15 years. He is comparing Vietnam veterans with their non-deployed siblings to determine whether biomarkers for PTSD represent a genetic risk factor or have been acquired as a result of exposure to a traumatic event. Based on his work, he cautioned: "Investigators can't just assume abnormalities they find in PTSD are caused by trauma. For instance, one of our studies showed that decreased size of the hippocampus, an area of the brain involved in learning and memory, was a familial trait, although other investigators have associated changes here with stress. It's the physiological responses, such as an increased heart rate after startling stimuli, that seem to be the most reliable acquired markers of PTSD."
Pitman noted that the most replicated neuroimaging finding in PTSD is a diminished activation of the prefrontal cortex. The theory is that this brain region fails to inhibit the amygdala, an emotional processing center in the brain, thereby preventing extinction of the intense emotional reaction to trauma. In fact, exposure therapy, in which an individual is gradually exposed to fear triggers in a safe setting, is known to be effective in treating PTSD symptoms in many cases. Pitman held out hope that promising drug interventions might come as researchers discover the molecular basis for the strengthened connections in the amygdala that seem to support the emotional response in PTSD.
Dr. Thomas Neylan, director of the Posttraumatic Stress Disorders Clinical and Research Programs at the San Francisco Veterans Affairs Medical Center, presented a discussion on the vital role sleep could play in recovery from injury. According to Neylan, sleeplessness is the most common complaint in both mild brain injury and PTSD, affecting quality of life and functioning. And, in what could be a vicious cycle, the frontal lobes of the brain -- those cognitive regions that can temper emotional reactions -- are negatively affected by sleep loss.
Because studies have shown that those with PTSD report sleep disturbances while objective measures of their sleep/wake patterns sometimes appear normal, Neylan hypothesizes that their brains are hyperaroused and vigilant even during sleep. He is exploring the possibility of promoting sleep by antagonizing the brain's receptors for corticotropin releasing factor, a type of neurotransmitter involved in anxiety-related arousal control. He hopes that his tests of a CRF antagonist may lead to safer sleep medications.
Another approach to helping those who are coping with brain dysfunction, regardless of the cause, was presented by Dr. Anthony Chen, director of the University of California's and VA's collaborative Program in Rehabilitation Neuroscience. His research focuses on theory-driven rehabilitation, developing targeted cognitive training along with ways to measure the outcomes.
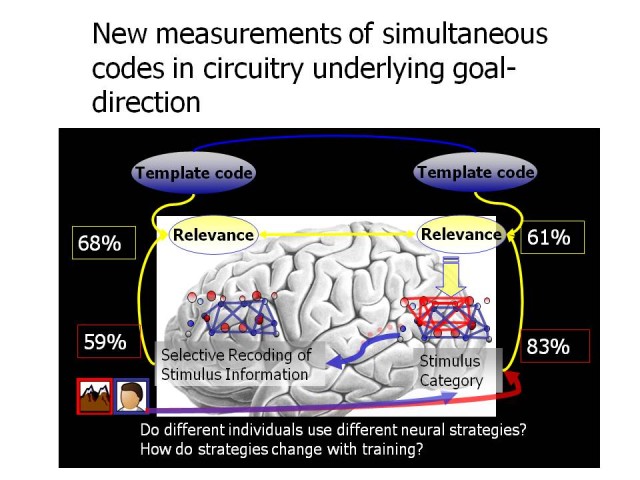
Because many individuals with physical or experiential brain injuries have difficulty with cognitive functions crucial for accomplishing goals (learning, paying attention, remembering and problem solving), his team developed training techniques to enhance goal-directed cognition. Chen is measuring effects through a combination of performance on neurocognitive tasks and real-world functional tasks, and determining neural mechanisms using functional magnetic resonance imaging biomarkers. By decoding the brain's cortical activity patterns, he is able to better understand the coordinated neural processes involved in goal-directed control, providing a foundation for developing more effective interventions to improve cognitive functioning.
TATRC partners with other USAMRMC units such as the Combat Casualty Care Research Program and the Military Operational Medicine Research Program to provide important leadership in military-focused medical research efforts in several areas. For more information on TATRC's research funding and collaborative opportunities, visit www.tatrc.org.

Social Sharing