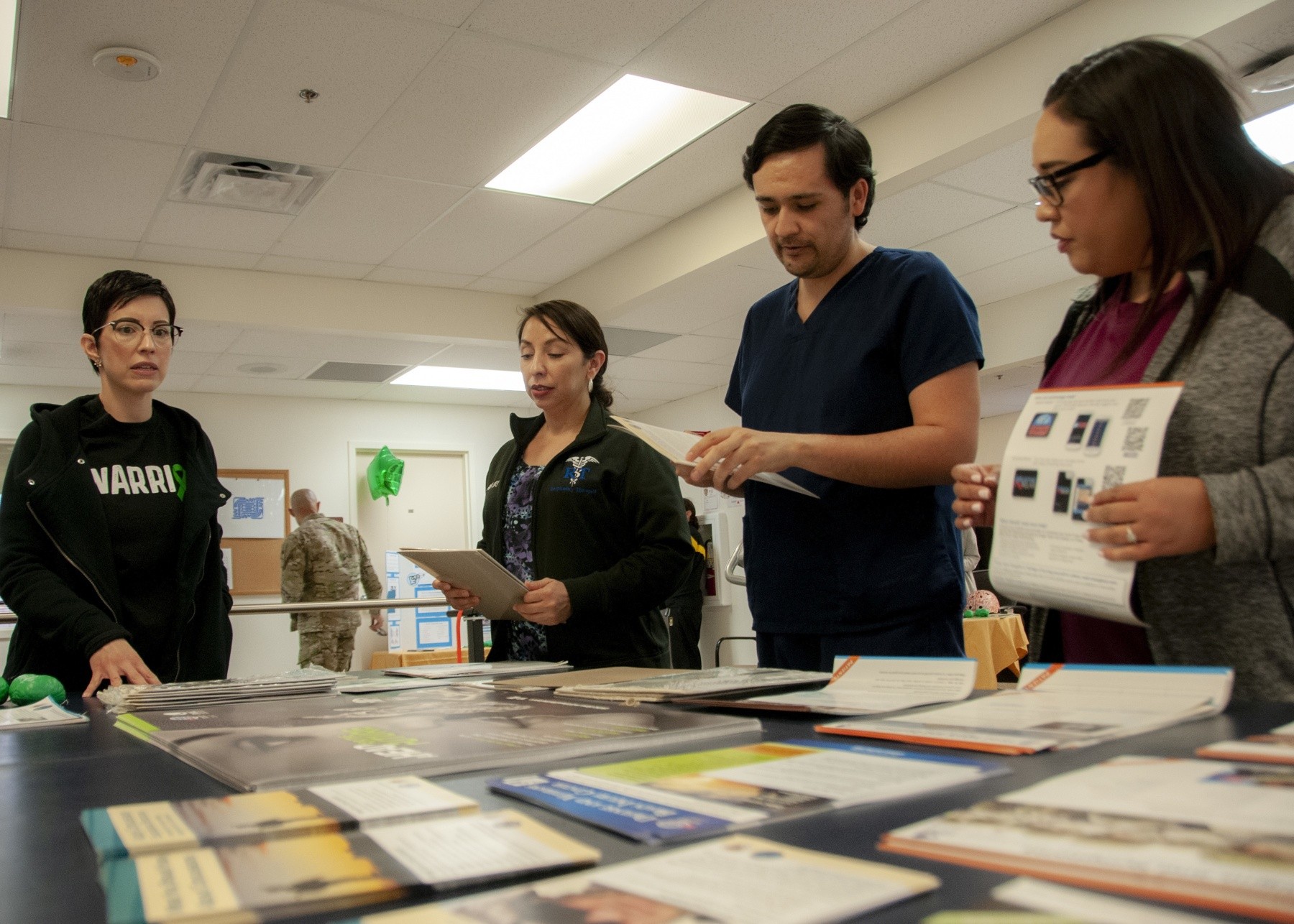
Each year, thousands of service members are diagnosed with Traumatic Brain Injury (TBI) with over 383,000 diagnosed since 2000, according to the Defense and Veterans Brain Injury Center (DVBIC). To raise awareness of treatment modalities, technology and the care available to service members and their families, and local veterans, the Fort Bliss TBI Clinic held an open house, March 29.
The event featured the clinic's different approaches to assessing, managing, and educating about TBI symptoms such as sleep disturbances, cognitive impairment and headaches to service members and their families. The event was held in observance of Brain Injury Awareness Month, which is observed annually during the month of March.
"The purpose (of the event) is to allow any individual to come in, it's normally a closed-off space, to see what we do here," said Dr. Sean Sebesta, chief, TBI Clinic, William Beaumont Army Medical Center. "(TBI) is a very complex system, with multiple issues that can all cause the same symptoms, or similar symptoms. That's what we're trying to show, it's not a simple service where you stop by for a tune up and go, it usually takes more than that."
Throughout history, TBI's have often been misunderstood. Ancient burials show evidence of trepanation, the surgical intervention of drilling a hole, in the skulls of combatants as attempts to relieve pressure from blood buildups caused by brain injuries. Modern understanding of TBI stem from various conflicts and including the wars in Iraq and Afghanistan, where roadside explosions were used extensively by insurgents, causing over 60 percent of all coalition casualties.
For Pfcs. MaeJean Ramnarace, and Cheyenne Bynes, both training to be medical laboratory specialists at WBAMC, the event stressed the advancement in TBI treatment, a condition neither had ever been exposed to before, other than hearing about it on television.
"It's nice to know we have these resources available, a lot of people don't have access to these types of resources, as Soldiers we are fortunate enough to have them readily available," said Ramnarace, a native of Honolulu. "Events like this, having an open house, gives people the education they need to know if (TBI) might affect them. There's a lot of problems that may come from TBIs and a lot of people may not know (the problems) stem from (TBI). If they are aware of the causes, they can treat the source instead of just treating the symptoms."
According to Claudia Mendoza, a speech language pathologist at the TBI clinic, the disruption of normal function of the brain caused by TBI are categorized as mild, moderate, severe and penetrating (open-head injury). Most mild brain injuries are also referred to as concussions, while more severe injuries may have a longer-lasting effect on individuals such as behavioral, functional or psychological changes.
Because symptoms vary and may affect various functions, the Fort Bliss TBI clinic provides a holistic approach to treating patients, including exercise, vision therapy, behavioral health, and even art therapy to aid in treatment.
"The concussions and TBIs that we see are often not understood to be as complex as they really are," said Sebesta, also the director for the Defense and Veterans Brain Injury Center at Fort Bliss. "One of the things when you have a concussion is you generally know it. But you don't know when you've just developed post-traumatic stress symptoms, chronic insomnia, hypervigilance, all those things are pretty normal in combat, to some degree, but they don't announce themselves as an entity or illness. These are issues that can cause problems for the rest of (patients') lives. We try to sort it out a little, more importantly, we try to (treat) all the aspects of care for all those different (symptoms) they have, by doing that we help out all of (the symptoms)."
According to Sebesta, the clinic utilizes a biopsychosocial model of health with a multidisciplinary approach to treating patients, through referrals to behavioral health, MRIs, and employment of psychologists, speech and vision experts and the Army base's only art therapist to assist patients with stress management. Additionally, the clinic conducts research specific to the Fort Bliss population.
Across the Military Health System, new clinical tools are being launched to help medical providers accurately diagnose, record and threat TBI through the Military Acute Concussion Evaluation 2 (MACE2) and concussion management tool, designed to improve concussion assessments and care.
In October 2018, then Deputy Secretary of Defense, Patrick Shanahan, recognized TBI as a less visible and poorly understood consequence of recent conflicts, while acknowledging the changes service members and their families struggle to understand when dealing with symptoms of TBI in all its forms. To counter TBI, the DOD has launched a comprehensive strategy and plan of action comprised of several elements including: Research; surveillance and prevention; diagnosis, treatment rehabilitation and reintegration; and outreach, education and training.
"We're really working together to create someone who is much improved by the time they leave this program," said Sebesta. "We're trying so many different aspects of care. We try to find the right treatment for the right person, if they're persistent and we're persistent then it usually it works out."





Social Sharing