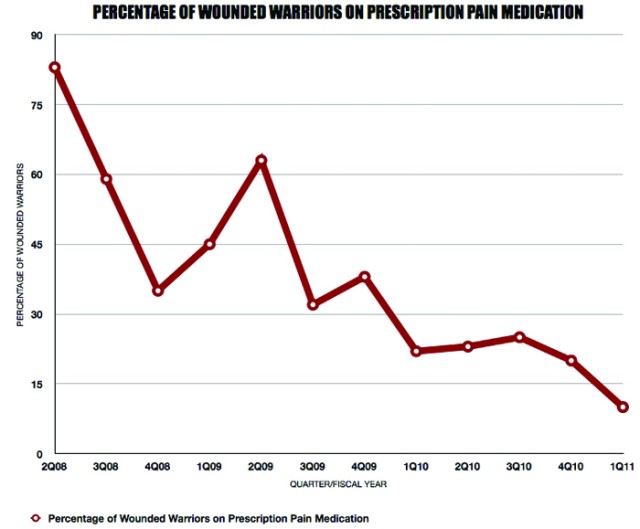
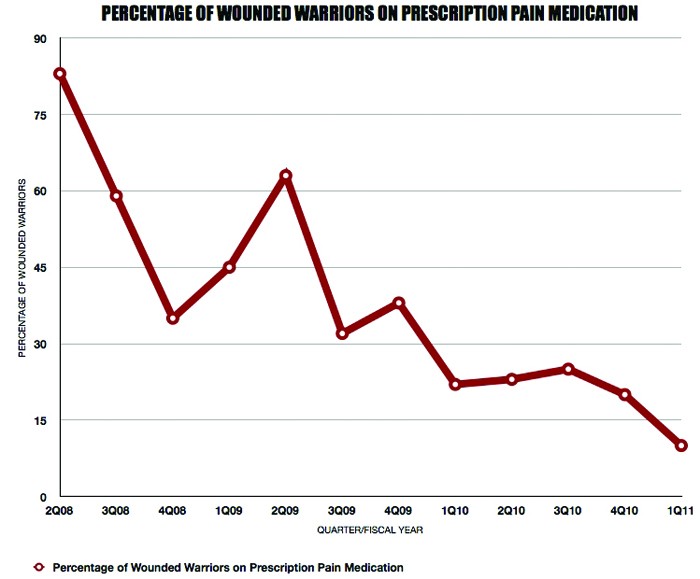
WASHINGTON, April 29, 2011 -- The pain management program offered in the Warrior Clinic at Walter Reed Army Medical Center has drastically reduced the number of Wounded Warriors receiving prescribed pain medication.
In 2008, roughly 83 percent of the Wounded Warriors assigned to Walter Reed's Warrior Transition Brigade were using prescribed narcotics. With the end of the first quarter of fiscal year 2011, that number had been reduced to 10.2 percent, according to officials.
With nearly 1,470 Wounded Warriors seen quarterly, the Warrior Clinic is taking a unique and steady approach to treating and educating Soldiers with pain.
Being the "Home of Warrior Care" has allowed Walter Reed Army Medical Center, or WRAMC, and the Warrior Clinic to establish many U.S. Army standards and even best practices for the care of Wounded Warriors throughout the military services.
"When they [Soldiers] get injured on the battlefield, and they come here as inpatients, we set them up to treat their pain," said Lt. Col. Sandra McNaughton, officer-in-charge, Warrior Clinic, WRAMC, Warrior Transition Brigade.
Often that requires heavy medication due to the nature and severity of their injuries. That medication can cause dependency and other adverse effects. Medically speaking, it's called "iatrogenic," which is describes as an illness or reaction caused by treatment from the medical profession and/or system.
"We would be practicing malpractice if we gave them a few Motrin or Tylenol to relieve their pain," said Col. Lisa Black, brigade surgeon, WRAMC, WTB. "So we looked to see how we could minimize risk and reduce the drug cocktails in Soldiers."
McNaughton and Black added that the Warrior Clinic and its primary care managers, supporting nurse case managers, social workers and pain management specialist understand as part of a Wounded Warrior's comprehensive treatment plan, they have a duty to help the Soldiers and transition them off pain medication.
With the support and direction of Navy Cmdr. Necia Williams, integrated anesthesia chief for National Naval Medical Center and Walter Reed, McNaughton and the Warrior Clinic staff initiated and incorporate a pain management program into the Warrior Clinic.
Pain is a continuum from acute to chronic pain. The challenge the Warrior Clinic faces is treating pain in the acute phase in the effort to prevent it from developing into chronic pain, according to Dr. Christopher Spevak, anesthesiologist and pain physician, Warrior Clinic, WRAMC.
What's unique is the way this team treats pain.
Concerning pain management, the Army Medical Command and the Warrior Clinic have adopted an integrated interdisciplinary approach to the treatment of combat related injuries.
They're looking at the whole person.
"It's a holistic, interdisplinary, and multi-modal approach. Pain management is not simply giving opioids," Spevak said. Opioids are medications that fall within a class-referred to as prescription narcotics, which includes Morphine, Codeine, Oxycodone, and related drugs.
According to Spevak, in the last couple of years research has shown that if you initially treat pain effectively you can prevent the rewiring of the brain and prevent chronic pain. Treating acute pain as close to the time of injury, with the appropriate medication is just one part of this multidisciplinary approach.
However, medications play an important role in the healing of these Soldiers.
"There are many ways to treat pain initially; opioids are part of the whole pie. We have regional techniques and we have gone forward right into the battlefield and placed regional catheters to infuse local anesthetics to numb the area," Spevak explained.
Using this concept, these specialists are battling a generational perception that's not just an issue in the military but across the board of, "take a pill."
The Warrior Clinic has devoted a significant amount of resources into looking at the alternative methods for managing and minimizing pain, from establishing complementary and alternative training sessions, offered every Monday, in Bldg. 2, Heaton Pavilion, in the Radiology Conference Rm. 1X37, to developing a whole curriculum of modalities that can help Soldiers with pain other than with medications.
This dynamic and holistic approach to addressing and treating pain uses a wide variety of resources that look at the mind, body, and cognitive behaviors of the Soldier as well as incorporating and educating the Soldiers families into the treatment and overall management of pain.
"We are very active in using acupuncture. That's a very big component of my practice, chiropractic modalities, through behavioral health we have specialized people that help with bio-feedback and even hypnosis," Spevak said.
Accountability of the organization and of the Soldiers is key to this success.
"We have an incredibly perceptive and bright [Wounded Warrior] population here in the Warrior Clinic," Spevak said.
However, it's not a perfect world, he explained, and this led to the development of the U.S. Army's Risk Mitigation Policy for the care of Wounded Warriors by the WRAMC WTB.
Key elements of the policy include appropriate tracking and monitoring of Soldiers and their medications, controlling quantities, prescribing the right medication at the right time and other aspects. Clinic staff also monitor the behavioral health of Soldiers and can identify "at risk" Soldiers, even those that have gone to the emergency room between visits to the clinic.
If necessary, they can ensure individuals enroll in the Army Substance Abuse Program and monitor Soldiers through random urine drug screens within the companies. Healthcare providers and WTB cadre are constantly reevaluating the Soldier to ensure there is continuity of care.
"The beauty of this program here that Lieutenant Colonel McNaughton has assembled is that it's within the footprint of the Warrior Clinic," Black said.
"It's nice because it's a one-stop-shop. We have the pharmacy. We have Electronic Medical Manage-ment Assist Pharmacist.We have trauma, and we have our pain management. Our nurses, primary care providers, and we're all one with the same focus, the warrior," McNaughton said.
This proximity allows for the providers at all levels to work and train together, creating a higher level of awareness.
Spevak, a civilian doctor and associate professor of anesthesiology from Georgetown University Medical Center, in Washington D.C., was recruited because of his specialization in anesthesia/pain management and has been instrumental in the collaboration with PCMs. They strategically placed him so that he can have direct access between the providers at all times and they can have direct access to him.
"They [PCMs] have learned a lot about how to manage these warriors and the pain treatment plan that is involved, and he [Spevak] has branched to inpatient as well," McNaughton said.
Black attributes their success to the closeness of the team and their focus. They're all looking out for each other and their patients, "because the warriors are our family too," she added.
Sharing their effort and best practices is also part of their success. The clinic frequently gets requests from across the pain management field to share and talk about their progress and they have even started to extend and integrate with the Department of Veteran Affairs and with civilian providers.
Last month, Lt. Gen. Eric B. Schoomaker, Army surgeon general and commanding general of the U.S. Army Medical Command; Brig. Gen. Richard W. Thomas, assistant surgeon general for force protection; Col. Kevin Galloway, chief of staff for the Army's Pain Management Task Force; and Col. Chester C. Buckenmaier, chief, Army Regional Anesthesia & Pain Management Initiative, Walter Reed Army Medical Center were honored with awards March 26, 2011, during the 27th annual meeting of the American Academy of Pain Medicine.
The Academy Presidential Commendations were presented for efforts toward improving comprehensive pain management through the U.S. Army's Pain Management Task Force - efforts that have ranged from better use of anesthesia to non-pharmacological treatments such as acupuncture, chiropractic therapy, yoga and biofeedback.
According to its charter, the Army Pain Management Task Force was established in August 2009 to make recommendations for a MEDCOM comprehensive pain management strategy to approach pain management holistically. The task force's multidisciplinary and multimodal approach aims to provide optimal and effective care of pain, while ensuring the quality of life and education of Soldiers and other patients with acute and chronic pain.
"Our mission is to educate the Soldier and the family members. We have the honor, duty and obligation to treat them in the best possible fashion," Spevak said.
For more information regarding the pain management program, contact the Warrior Clinic at (202) 782-9822 or 23.
Related Links:
Army Medicine leaders honored for Pain Management efforts
VIDEO: Pain Management Task Force


Social Sharing