WASHINGTON (Army News Service, June 21, 2013) -- This week, the military medical community was notified that a new antibiotic drug is now available to treat Soldiers who have life-threatening, multidrug resistant bacterial infections.
Arbekacin is a new antibiotic treatment for multidrug resistant, or MDR, infections. Those types of infections may complicate wounds sustained by Soldiers in theater, said Col. Michael Zapor, an infectious diseases physician at Walter Reed National Military Medical Center, in Bethesda, Md.
STOPPING A KILLER
"Of all the bacterial species found on the planet, relatively few are intrinsically multi-drug resistant pathogens," Zapor said. "In Iraq and Afghanistan, the bacterium known as Acinetobacter is one such MDR bacterium that has caused problems in our patient population."
Acinetobacter is commonly found in the water and soil of regions such as Iraq and Afghanistan, he said. Although it's intrinsically resistant to many antibiotics, it's not especially virulent and generally not problematic in humans unless their immune system has been severely compromised or the bacterium is inoculated deep into macerated tissue, as would occur with massive open wounds resulting from battle injuries.
Infections caused by the bacterium were prevalent during the Vietnam War, he said. But at the time, Acinetobacter remained mostly susceptible to antibiotics.
However, over time, resistance emerged and antibiotics became less effective against many pathogenic bacteria, including Acinetobacter.
"We're losing antibiotics much faster than new ones are coming through the pipeline and made commercially available," he explained. "In the 1950s, penicillin cured a lot of bacterial infections. Not so now."
Humans reproduce at around 20 years, he said, but bacteria reproduce maybe every 20 minutes. With prolonged exposure to antibiotics, they evolve over time to become drug resistant, he explained. They're survivors.
"Now, our Acinetobacter isolates are resistant to most antibiotics," he continued. "It's only a matter of time before pan-resistance emerges", thus, the urgency for a new antibiotic.
SLOW PROCESS
In 2004, when Zapor was a battalion surgeon with the 10th Mountain Division in Iraq, he and colleagues started seeing cases of Acinetobacter and knew that a new antibiotic was needed, and soon.
At the time, he said, Arbekacin was being used in Japan for the treatment of pneumonia and septicemia caused by methicillin-resistant Staphylococcus aureus, or MRSA. Zapor thought the drug might have promise for treating infections caused by other MDR bacteria, to include Acinetobacter.
Lab trials were initiated at Walter Reed, and Arbekacin was found to be effective against many isolates of Acinetobacter, as well as other potentially harmful bacteria like E. coli, Klebsiella pneumoniae, Enterobacter and Pseudomonas aeruginosa, as well as MRSA. The next step was to get it approved for use in humans.
Zapor drafted a human-use protocol with the U.S. Army Medical Materiel Development Activity, or USAMMDA, as a sponsor. As the drug's principle investigator, Zapor was responsible for shepherding Arbekacin through the federal regulatory process for approving new drugs. It was harder than he ever imagined, he said.
Surprisingly, the Food and Drug Administration was very receptive to a human-use protocol and encouraged his team to proceed, he said. But progress got mired down in scientific and institutional reviews and many painstaking revisions to the protocol were required.
The process dragged on for years, but he finally got the green light to proceed with the human-use protocol this month. Meanwhile, Soldiers wounded in Afghanistan continued to develop MDR infections.
"Isn't it ironic that approval was finally given at a time when the war is winding down and our population of wounded warriors is shrinking?" he said.
But Zapor said he knows regulators need to ensure drugs are safe for use, adding that the Department of Health and Human Services and Congress are very aware that the process should and could be better streamlined. Moreover, pathogens will invariably become more drug resistant and Arbekacin remains available for future use.
WAITING TO POP THE CORK
Zapor said he and the protocol's sponsors at USAMMDA intend to celebrate as soon as the first patient with an MDR bacterial infection is successfully treated with Arbekacin.
As of yet, however, no one has received treatment with Arbekacin. This is due to the protocol's intentionally strict eligibility requirements, designed to delay the emergence of Arbekacin resistance, he said.
Eligible patients include those with MDR infections of the lungs, urinary tract, soft tissues, skin, bones and blood, for whom other antibiotics are either ineffective or contraindicated. That means other antibiotics either won't work or produce undesirable side effects like allergic reactions, he said.
Also, the treatment will only be available at Walter Reed. This way, use of the antibiotic will be tightly regulated, minimizing the risk of the emergence of drug resistance.
Fortunately, there are far fewer war wounded these days so "we anticipate an infrequent need for Arbekacin at this time," he said.
Moreover, fewer Soldiers who get wounded are being infected with Acinetobacter, he said. The causes of this are probably multifactorial. For example, during the early part of the war, it was common practice to place wounded Iraqi and U.S. Soldiers side-by-side in intensive care units.
"However, we learned that the wounded Iraqi soldiers tended to be colonized with Acinetobacter" at a much higher rate than were the Americans, he said. "One possible scenario is that as doctors and nurses moved from bed to bed, they might have unintentionally transmitted the bacterium between patients.
"Over time, the indigenous wounded were separated from the American wounded and the prevalence of Acinetobacter colonization among the latter declined," he continued.
IMPORTANCE OF ARMY MEDICINE
Without the support of Army medicine, it's doubtful Arbekacin would have ever been tested for use against MDR bacteria, he said. The Japanese, who licensed Arbekacin in the early 1990s, approved it for use against MRSA. Although there were scattered reports of efficacy against other organisms, no role was envisioned for its use against MDR bacteria.
The Japanese were, however, very helpful in translating documents relating to their early studies into English for us, Zapor said.
"I truly think they were motivated by humanitarian reasons and an appreciation for our problem with MDR infections in our war wounded," Zapor said.
Moreover, the drug's manufacturer, Meiji Seika Pharma Corporation, has agreed to supply Arbekacin for the protocol at no cost.
Zapor said in the U.S. there was not much commercial incentive for the kind of research he and his team did with Arbekacin. But Army medicine, he said, sees an incentive when battlefield injuries and illness dictate the need for a new drug or product.
Examples of that include the anthrax and hepatitis A vaccines, treatments for malaria, clotting bandages and recent improvements to devices like prosthetics and the Combat Application Tourniquet.
Zapor predicted that drugs for hard-to-treat fungal infections of wounds which are also problematic in wounded warriors will be the next candidates for new drug studies.
More potent and resistant pathogens are emerging all the time, he said, explaining there won't be any shortage of new work to do.
Just this April, for instance, a new virus, the MERS-CoV, was reported in Saudi Arabia. The fatality rate is around 65 percent, according to researchers at Johns Hopkins.
Someday, he said, Arbekacin resistance will emerge and the usefulness of that drug will be limited. "We're just hoping to stave off the inevitable."
MALARIA
When Zapor was serving in Iraq, he said he didn't see a single case of malaria except in those who had contracted it elsewhere.
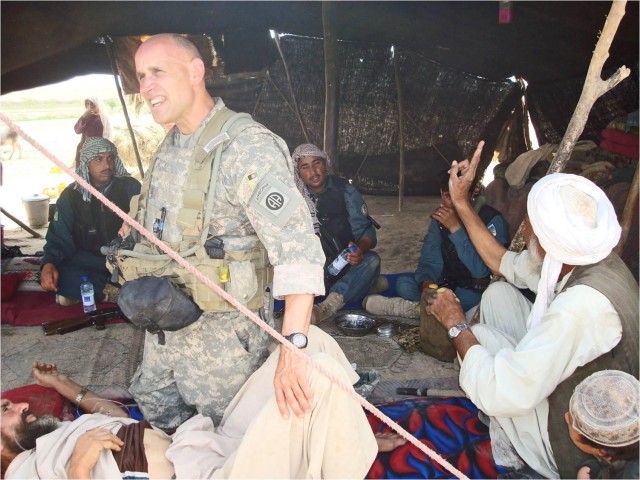
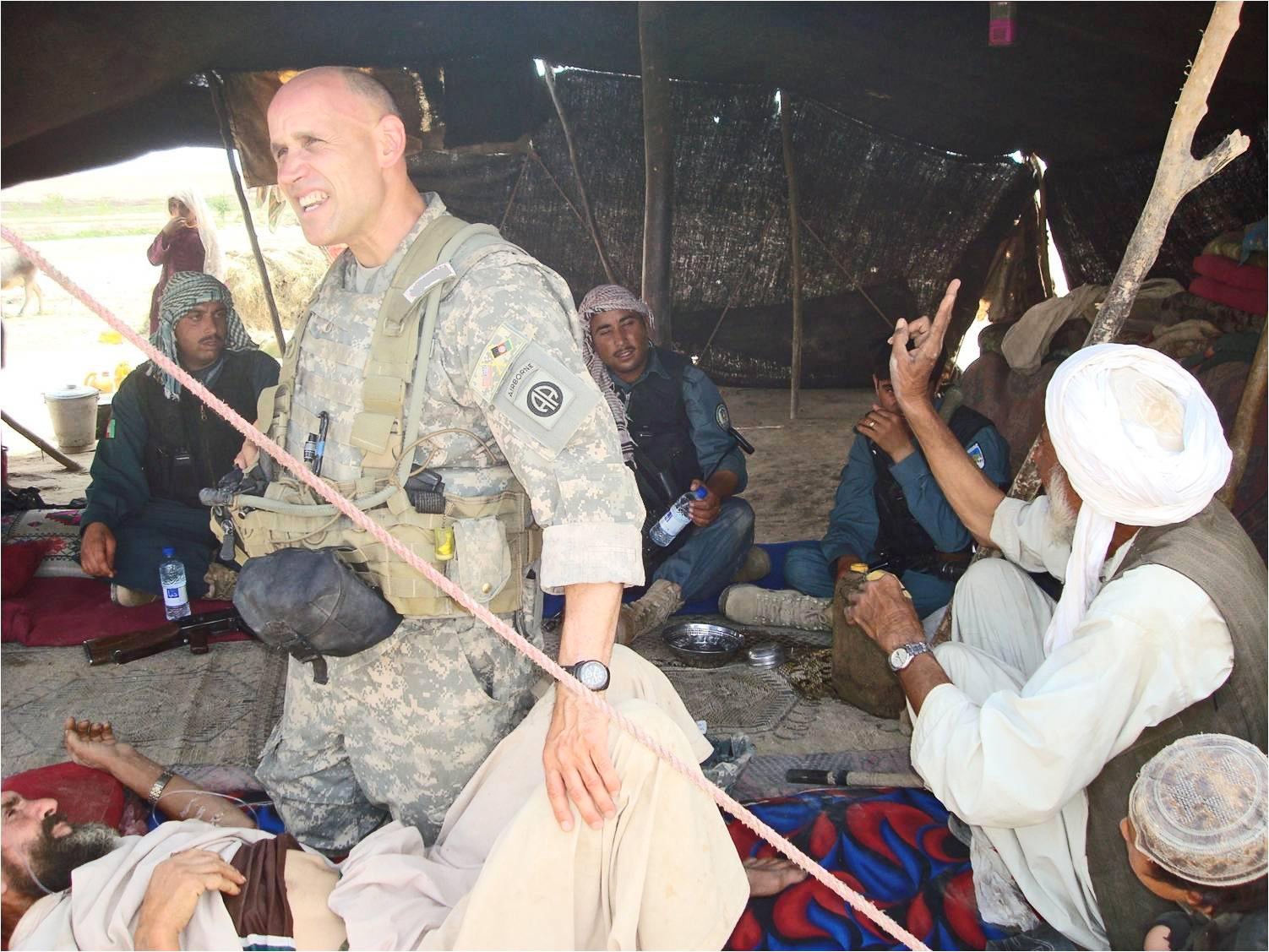
That was not the case when he was deployed to Afghanistan in 2010, as a battalion surgeon with the 82nd Airborne Division.
"There is a lot of malaria there," he said.
There are five species of clinically relevant malaria in the world, he said, and Plasmodium vivax is the one most commonly found in Afghanistan. Although not as dangerous as the deadly Plasmodium falciparum, P. vivax can cause serious illness. Moreover, if inadequately treated, P. vivax infections can relapse.
Drug resistant malaria isn't widespread in Afghanistan. In most cases in which Soldiers are diagnosed, they did not comply with directives to take anti-malarial medication, he said. Also, some were not applying insect repellent or it became ineffective due to heavy sweating.
Q FEVER
The illness "Q fever" is caused by inhalation of the Coxiella burnetii bacteria, found in the feces of birds and other animals as well as the placenta and amniotic fluids from birthing animals. The bacteria become airborne, usually by latching on to dust particles.
Acute infection is characterized by pneumonia and liver inflammation. Chronic infection may result in damage to the heart valves, Zapor said.
"Q fever is probably one of the more vexing infections we've had to deal with among troops returning from Iraq and Afghanistan," he said.
The reason, he explained, is that it is difficult to diagnose. Patients appear to have pneumonia, he said, and physicians may not suspect Q fever unless they also are able to detect damage to the liver and put the two together.
Once suspected, it is very difficult to definitively diagnose, he said, noting that there are only a few specialized labs that test for it and there may be discordance in results.
"You can get two different results from two labs," he said, adding that several years ago colleagues in the Armed Forces Infectious Diseases Society came up with guidelines in an effort to provide guidance for military physicians on diagnosing and treating patients with Q fever.
Unlike most other bacteria, C. burnetii is fastidious and cannot be grown in hospital laboratories. Instead, diagnosis involves looking for the presence of surrogate markers of infection, Coxiella burnetii antibodies in the blood, he said. However, there are several types of C. burnetii antibodies corresponding to different phases of the bacterium's growth and their levels rise and fall over time, confounding the interpretation of test results.
Patients who have suffered from Q fever can also suffer additional complications that come a result of the infection. One such example is damage to the heart valves, Zapor said.
Because of this, "there has been a lot of discussion in the military infectious diseases community about whether or not to test every Soldier coming back from theater or only those with respiratory infections," Zapor said.
Zapor said C. burnetii is found in the U.S., but Q fever is probably under-reported here. When it is diagnosed, it is usually in someone with an occupation that puts them at increased risk, such as veterinarians and farm workers.
BAGHDAD BOILS
A curious thing started happening when troops began arriving in Iraq and Afghanistan early in the war. Tiny sand flies were biting Soldiers who would then develop ulcerated skin sores, Zapor said.
As one can imagine, Soldiers who got these sores were alarmed, as were their commanders, who medically evacuated them, he said. Hundreds of Soldiers had their tours cut short by what they called the "Baghdad boil."
Actually, the disease is Old World leishmaniasis, caused by the Leishmania parasite and transmitted by sand flies, Zapor said.
Leishmaniasis was common among Soldiers serving in the Mediterranean and North Africa during World War II, but "over time, it was forgotten by the collective consciousness," he said.
The good news, he said, is that the disease is usually painless and clears up on its own without treatment.
As commanders came to realize that the threat was less ominous than originally supposed, he said, they opted to monitor those affected in theater instead of sending them stateside.
Over time, the incidence of the disease diminished. That was a result of improved living conditions for Soldiers, including sleeping quarters with air conditioning. With fewer Soldiers sleeping on the ground at night, fewer were exposed to the sand fly that carries the parasite.
As Soldiers deploy worldwide in regionally aligned units, Zapor said new pathogens will be discovered, and old pathogens will again rear their heads. Army medicine, he said, will be there to protect them.
Related Links:
Army to honor doctor for fighting deadly viruses
Social Sharing