FORT BRAGG, N.C. -- While carrying a ruck sack may sometimes feel like the equivalent of carrying a refrigerator on your back, a ruck sack is not able to provide a stable, temperature-controlled environment for lifesaving blood products that might be needed in remote or deployed environments.
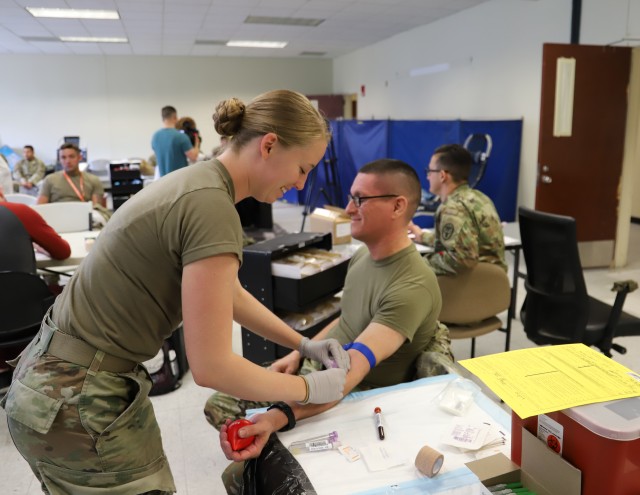
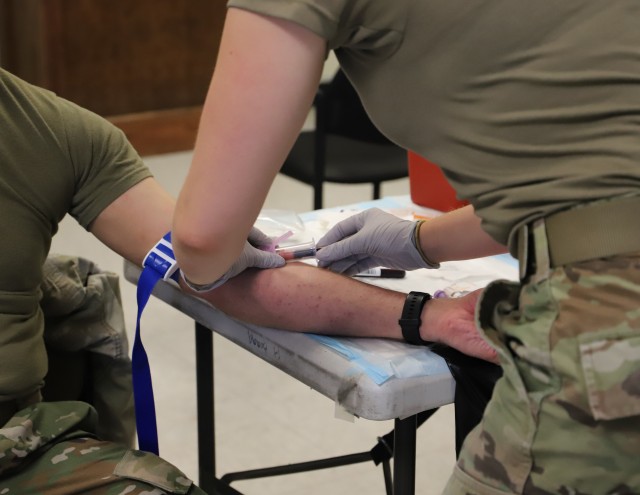
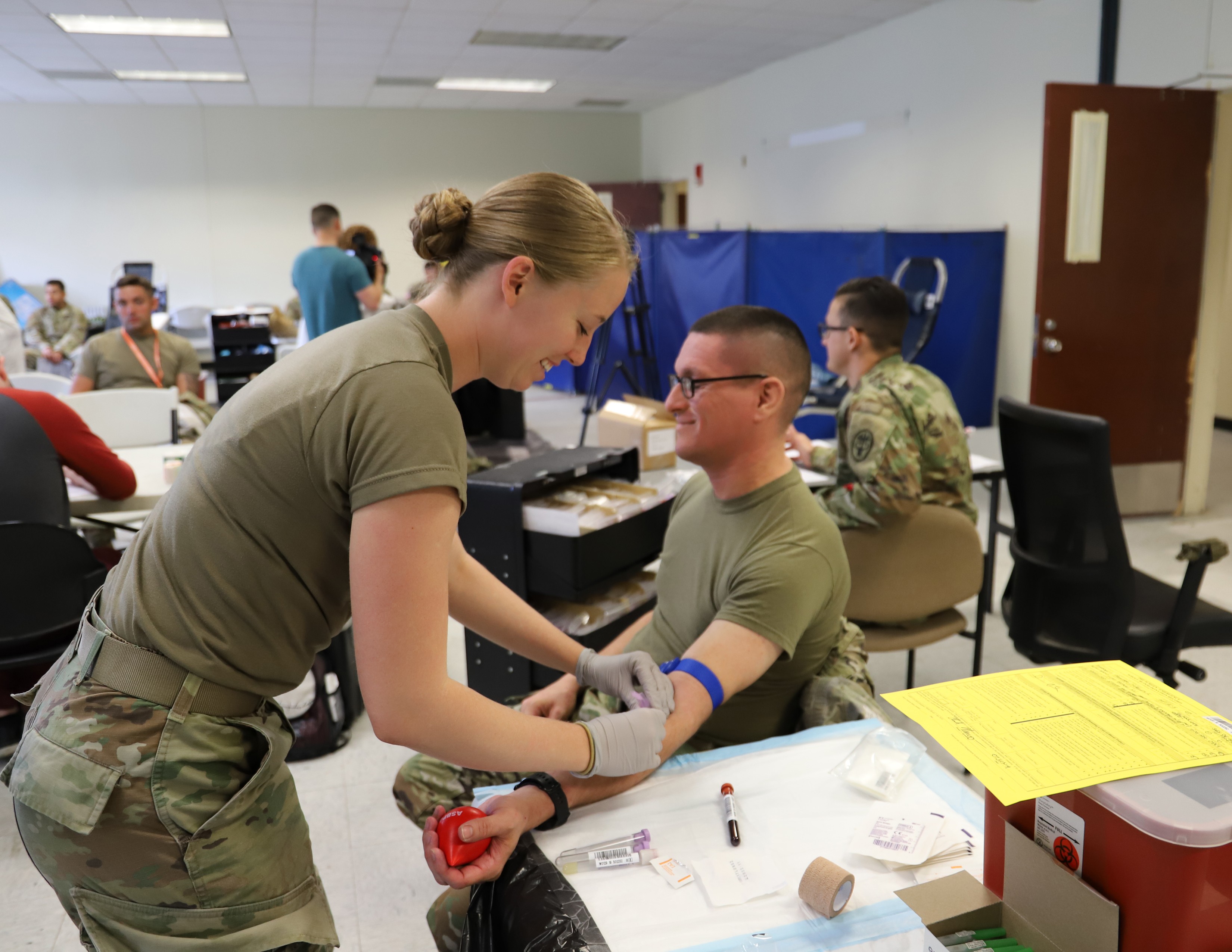
The XVIII Airborne Corps and the Armed Services Blood Program are partnering to identify Soldiers with blood type O who have low levels of antibodies in their blood. These individuals have the ability to provide an immediate blood donation to an injured person of any blood type that needs a transfusion at or near the point of injury.
"We are taking individuals with type O blood, who are already considered universal donors for packed red blood cells, and testing the levels of antibodies in their blood," said Lt. Col. Melanie Sloan, director, Fort Bragg Blood Donor Center. "Everyone has antibodies. They are naturally occurring and can attach themselves to transfused blood cells. The titer testing helps identify individuals with lower levels of these antibodies."
The Army is currently using the standard of 1 to 256 for the level of antibodies in the individuals identified as low titer O. When a person with blood type A or B needs blood and is receiving blood from a type O donor, the lower level of antibodies will make it easier for the body to accept the different blood type. Low titer O blood can be given to anyone in need, regardless of their blood type.
1st Lt. Robert Blough, the physician assistant for the 82nd Airborne Division Artillery (DIVARTY) and a former Special Forces medical sergeant, arranged for Soldiers in his unit to get tested for low titer O and also helps with mobile training teams to teach others how to perform field blood transfusions. He said he is passionate about implementing this program across the force because he has seen first-hand how it can save a life.
"In 2007, I had an Iraqi get shot in lower abdominal area," said Blough. "He was bleeding out internally, not overly fast, but there was nothing I could do to stop the bleeding inside him. The MEDEVAC got delayed. We were sitting on a mountaintop with this guy and I did not have the ability to transfuse blood to save his life."
Blough said that experience led him to volunteer for the working group spearheading the efforts to identify and screen fresh whole blood donors within the XVIII Abn. Corps.
The ability to transfuse blood while on the battlefield or at a remote location is hardly new and its effectiveness has been proven throughout history.
"We were doing this in 1918 during World War I," said Lt. Col. George Barbee, deputy corps surgeon, Task Force Dragon, XVIII Abn. Corps. "We were still doing whole blood transfusions in World War II up through the conflicts in Korea and Vietnam."
Barbee said that the Army transitioned from whole blood to component therapy in the 1970s. He said that while breaking the blood down into components is effective for treatment of some disease processes, it's not a feasible option for an immediate need for blood in the field.
"We have done a lot of studies to see what the best method was for saving lives through transfusion," he said. "They pointed back to whole blood."
The ability to identify low titer O Soldiers provides an agile and flexible approach to accessing the lifesaving measures that whole blood provides. The ASBP is increasing the amount of low titer O whole blood that it stocks on its shelves for rapid deployment and emergency measures.
However, blood needs to be stored in a temperature-controlled environment and bags of blood are not always readily available in a time of crisis. The pre-screened and identified Soldiers provide an instant supply if one of their peers is injured and needs a transfusion.
Each of the identified Soldiers is regularly tested for a variety of blood-borne diseases to ensure their safety and the safety of others. Patient privacy still applies for identified donors. If they are removed from the roster, the information is kept confidential and only revealed to the patient.
While the identification of being a "walking blood bank" might seem a little odd for the Soldiers who have this universal blood type, they are instrumental to efforts to improve survivability and mobility for the Army. Barbee hopes to someday see the program implemented across the Department of Defense.
"We completely support the XVIII Airborne Corps' whole blood initiative," said Col. John J. Melvin, chief nurse and chief of clinical operations, U.S. Army Forces Command Surgeon's Office. "It closes the gaps that we see on the battlefield for blood supply at role one and conditions of prolonged field care. In order to provide the best opportunity of survival for our Soldiers, the whole blood program is essential for our successful treatment of combat casualties."



Social Sharing