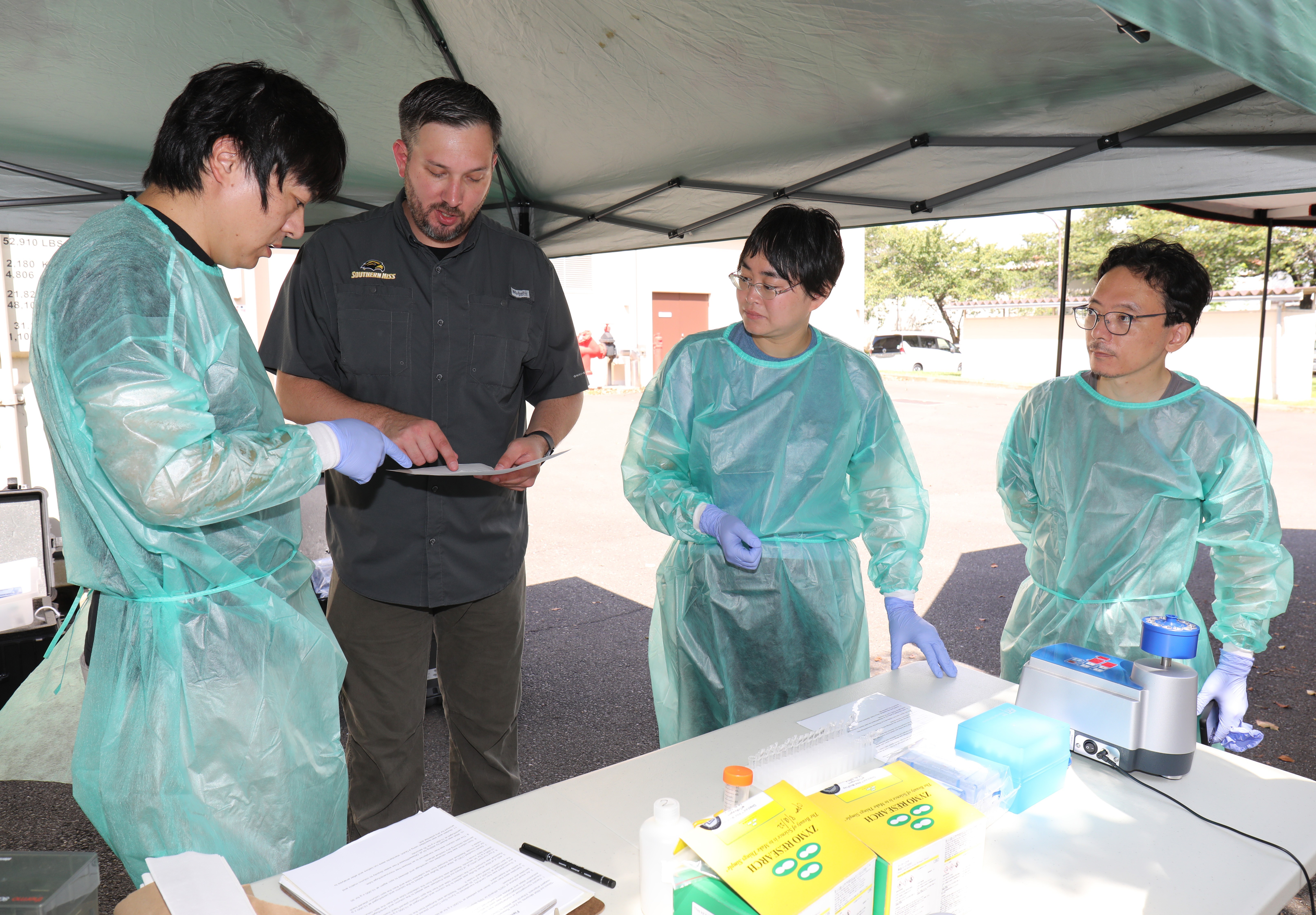
CAMP ZAMA, Japan – Experts from Public Health Command–Pacific demonstrated field lab techniques to Japanese counterparts and students during a knowledge-sharing event here Monday.
Specializing in molecular biology and entomology, the experts showed a handful of professors from the National Defense Medical College and interns in U.S. Army Garrison Japan’s summer internship program how to perform real-time pathogen analysis and discovery in an austere setting.
The event was part of an ongoing partnership with NDMC, which conducts research and trains current and future medical doctors in the Japan Ground Self-Defense Force.
“Without these partnerships and these networks, we would always be a step behind,” said Dr. Gary Crispell, chief of the Environmental Molecular Biology Laboratory here.
In 2019, Crispell’s lab joined the entomology lab to develop the concept of a pre-exercise mission that captures and tests vectors in training ranges ahead of major exercises in the Indo-Pacific region as a way to improve mitigation efforts against infectious diseases.
The labs went on to successfully demonstrate the concept in Okinawa. This summer, they applied some lessons learned, which included solar panels for power and lighter equipment to make the labs more mobile, and executed another mission before the Talisman Sabre exercise in Australia.
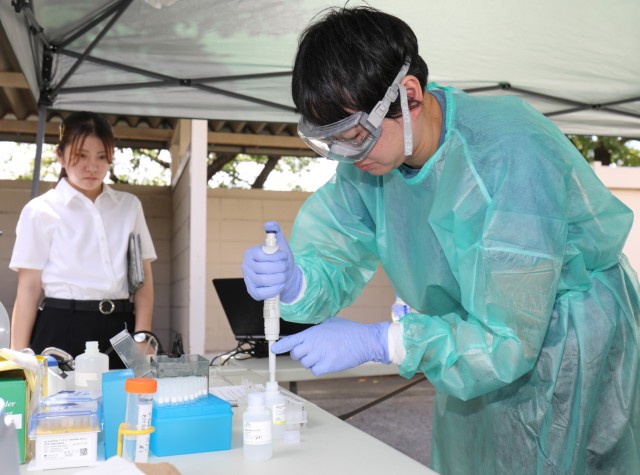
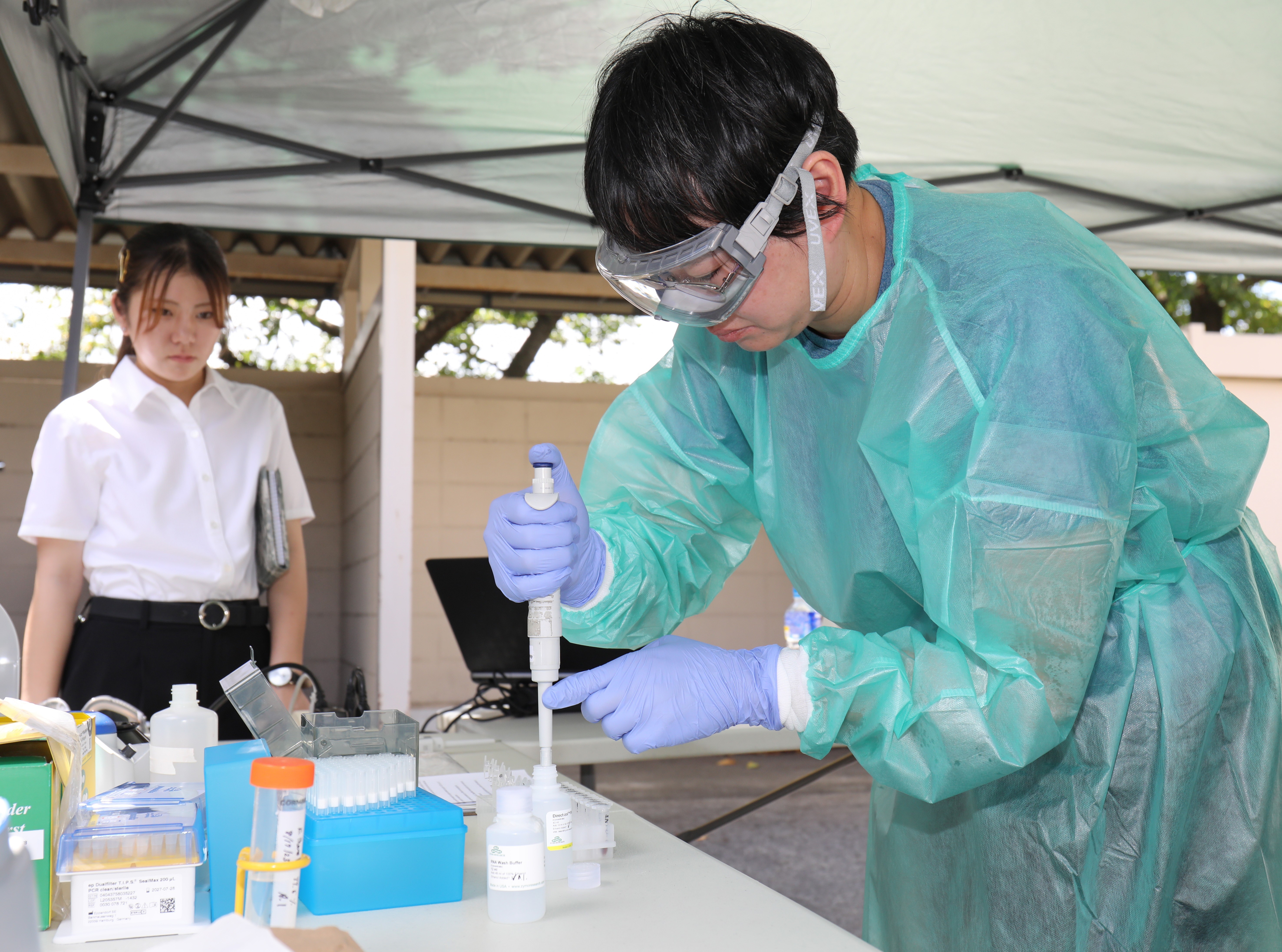
In Monday’s event, NDMC professors had the opportunity to receive hands-on training on the field equipment using mosquito specimens.
“We’re showing them, at the ground level, what we’re doing and what we’re using,” said Capt. John Eads, chief of the Entomology Laboratory.
Eads added the professors have also taught U.S. Army lab staff on how they collect and test for scrub typhus, a mite-borne disease in Japan.
Dr. Koki Kaku, director of Division of Infectious Diseases Epidemiology and Control at NDMC, said the event was the third time his team has trained with the Army labs. He said these bilateral engagements are beneficial, because both organizations have the same purpose — to protect service members.
“We have a friendly partnership,” he said, “so we want to join and study and research in this field together.”
Kaku said his team identifies pathogens inside their facility, so the opportunity to see how it can be done in the outdoors was helpful.
“This is a field operation, so we really want to know how to do this,” he said, adding they need to conduct this type of research at training ranges in Okinawa. “So this kind of practice is very important for us.”
Justin Nakamura, an intern who plans to study biomedical engineering at Dartmouth College in New Hampshire, said the field lab training was a unique experience for him.
While in college, he said, students learn about DNA, genetics and similar subjects, but an academic setting can be different from what happens in a working lab.
“You learn the fundamentals, but that doesn’t mean you can do this,” he said. “And so I think it’s more important, if you want to do any kind of job like this in the future, to actually get in the workplace and do it.”
The field lab project, which is funded by the Department of Defense’s Global Emerging Infections Surveillance program, or GEIS, aims to identify medical threats and provide current data on an exercise location.
Units sometimes do not deploy with vector surveillance equipment, Eads said, and may only bring gear that tests the water or soil, or measures the levels of noise personnel will be exposed to in the area.
Instead, they rely on vector and pathogen lists that could be out of date, as infectious diseases can evolve or be introduced to an area over time.
“A lot of the information we have is historical,” Eads said. “It’s not real-time relevant to where the medical planners can really develop a mitigating plan to ensure that the warfighters are protected once they go into the exercise location.”
Mitigation steps can include permethrin-treated uniforms, bed netting and insect repellant, he added.
Depending on the season and the size of a training area, the entomology team will capture thousands of mosquitoes, ticks or mites that the mobile molecular biology lab can then choose from for its testing.
“We really have to be in direct communication with the molecular team, so we know what we’re testing [for],” Eads said. “We’ll hand them off in a continuous cycle … and within 24 to 48 hours we know if a pathogen is present in that training area.”
Once an individual specimen is ready for testing, the process to determine if it is carrying an infectious disease can take up to two hours, Crispell said.
Before Talisman Sabre, for instance, lab technicians discovered some tick-borne diseases while their Australian counterparts found alphaviruses, such as Ross River Virus, which is transmitted by infected mosquitoes.
The two teams used a mic PCR machine, a small thermal cycle, that sped up the identification process and helped them quickly share the results with each other.
“We shared the data, so both sides had a picture, [which is important] because we were involved in the exercise together,” Crispell said.
As their team is the only one in the U.S. Army currently doing these pre-exercise missions, Eads said they will continue to publish information, including the equipment they use, on the GEIS network to help other units around the world do the same.
“We’re very transparent and trying to get it to catch on,” he said. “Hopefully it’ll keep the momentum and we’ll be able to standardize this program.”
Related links:







Social Sharing