Abstract
Recent shifts in medical personnel authorizations within Army organizations resulted in changes to the administrative control and assignment of medical personnel. Structural and doctrinal distribution of medical personnel changed from a 40-year-old system that provided medical resources in support of deployed forces. As a result, mechanisms to ensure skill maintenance through case-mix and quantity now require markedly increased coordination to prevent further deterioration. Clinical quality management, including assignment and talent management, became more difficult because of increased communication gaps.
The DOD acquisitions process provides a means of generating a solution that will sustain medical readiness, improve clinical quality management, and further automation of current manual processes. The first step in this process requires validation of the need. Validation provides entry into the acquisitions process. Planning further, an incrementally deployed software-based integration of nine separate systems of record (SOR) is one solution that meets the identified need and provides additional functionality.
Because validation is the gateway into the acquisition process, I focus on building a common operational picture (COP) to communicate the impact of the unmet need. I discuss the structure, organization, and policy affecting medical personnel management to provide context for the need. I provide for the way ahead with a framework for solution development within the acquisition process.
Purpose
Clinical quality management requires a continuous and objective assessment of individual and institutional performance. This assessment provides the detail necessary for holistic management of Army medical personnel, especially those assigned to operational units with duty in military treatment facilities (MTFs). Currently, the Army cannot effectively provide this assessment, identified as an urgent operational need (UON). The Army can fulfill the UON through the integration of multiple SORs. SORs possess the authority to store data and may also access the data stored in other systems.
The identified UON occurred recently with the shift of medical authorizations, directed by Headquarters, Department of the Army Execute Order (EXORD) 043-19. This EXORD created new conditions and systems for the administrative control of medical personnel and increased the difficulty of tracking personnel availability and skills maintenance. These elements are distinct from established Army doctrinal practices for physicians, given that the evaluation, treatment, and especially medical decision making, are not doctrinally prescribed.
This paper focuses on discussion of the background conditions which generated the UON. This focus provides a COP that supports validation of the UON. Throughout the discussion, I present the current disparate state of SOR functionality as related to the scope of clinical quality management. As a way ahead, I conclude with a proposed solution to meet the UON. Each SOR is complex, and discussion of their high-level interactions is necessarily brief. As a result, any omissions or errors in this discussion are entirely my fault, and open to correction.
Discussion
Personnel management and acquisitions are complex systems with diverse requirements and areas of expertise. This section provides a basic overview of key elements and policies to build a COP which enables further discussion of requirements and solutions. The COP requires discussion of Army organization and policy, the DOD acquisitions process, and use cases for key stakeholders, identified as the Defense Health Agency (DHA), Army Forces Command (FORSCOM), and Army Medical Command (MEDCOM).
Army Organization and Policy
Unit manning documents establish capabilities for specified functions through a given number and type of personnel and equipment. The two types of relevant manning documents are the Modified Table of Organization and Equipment (MTOE) and the Table of Distribution and Allowances (TDA). The MTOE is an authorization document for personnel and equipment, establishing requirements given a specific doctrinal mission. Each MTOE derives from a table of organization and equipment (TOE), with modification to meet specific mission requirements. A TDA document provides organizational structure and authorizations for a unit that does not have a TOE. TDA units are generally non-deployable. Currently, TDA documents establish the manning for fixed MTFs. The electronic military personnel office (eMILPO) provides the system for the management of individuals assigned to TDA units.
The manning documents reflect the varying availability of personnel and provide mechanisms to increase the manning. Both tables have columns for authorized and required personnel, with the authorized column based on the number of available personnel, equal to or less than the required column. The unit receives manning to required levels when performing their assigned mission, as opposed to training for the mission, usually in a deployed status. TDA units adjust manning based on workload, using the Defense Medical Human Resource System internet (DMHRSi) to compile self-reported work-center allocated time. The Digital Training Management System (DTMS) is the SOR that allows management of each Soldier’s training status. The Defense Readiness Reporting System-Army (DRRS-A) allows reporting and tracking of unit readiness.
The Army organizes its uniformed licensed physicians as officers, administratively organized under the Medical Corps of the Army Medical Department (AMEDD). As with all Army officers, physicians organize into areas of concentration (AOC), with assignment along specialty training. As an example, the AOC 61H denotes a family physician while 61J denotes a general surgeon. Regardless of specialty, the Joint Centralized Credentials Quality Assurance System (JCCQAS) provides management of credentials and privileges for each clinician associated with a given MTF. Before November 2018, manning policy assigned most physicians to TDA units. The MTOE for units requiring medical support when executing their mission reflected zero authorized positions and one, or more, required positions.
Developed in 1980, the AMEDD Professional Officer Filler System (PROFIS) designated qualified individuals in TDA assignments for temporary attachment to an MTOE unit for deployment. The PROFIS Automation System managed validated personnel requests, or taskings, to meet the MTOE requirements. Due to varying practice environments, both at home and deployed, length of deployment, and individual medical readiness, execution of the PROFIS met many difficulties. These difficulties included poor communication between physicians and MTOE units, multiple changes in PROFIS personnel during deployment, a decrease in case-mix complexity and technical skills, and many more.
For all Army personnel, including medical personnel who provide input, the Medical Operational Data System (MODS) tracks medical readiness including immunizations, administrative readiness assessments, work limitations, and more to provide individual readiness status. Conditions such as pregnancy or asthma limit deployability and increase the complexity of PROFIS administration. Although the electronic health record (EHR) documents the medical assessment, there is no connection of that SOR with MODS. There is also no current methodology to assess performed procedures and medical competency through EHR documentation. These administrative hurdles were further complicated by changes in healthcare administrative authorities.
The National Defense Authorization Act for fiscal year 2017 directed the transfer of administration of MTFs from the services to the DHA. In November 2018, the Department of the Army directed the transfer of 1,685 medical authorizations from TDA to MTOE units “to ensure the Army retains the ability to meet the operational medical requirements of combatant commanders and the national defense strategy.” These authorizations included Nurse Corps officers as well as Medical Corps officers, with the affected personnel designated as MTOE assigned personnel (MAP). Effectively, the affected medical personnel would continue to work at their previously assigned MTF while shifting administrative control to an MTOE unit, mostly commanded by non-medical personnel. The medical MTOE units, such as field hospitals and combat support hospitals, received the largest number of authorizations. Notably, these MTOE medical organizations do not routinely provide medical care until deployed, with training focusing on larger unit functionality such as logistics and movement.
Changing assignments to match the changed authorizations left most individuals in the same MTF job, primary care manager, surgeon, residency faculty, or department chair, but shifted administrative control to a unit external to the hospital, introducing required training and administrative events outside the control and purview of the MTF. Hospital commanders must coordinate with multiple units outside their chain of command, performing a wide array of missions, occasionally geographically separated across states. The MTF also loses administrative control and oversight for personnel actions, such as leave. These changes increase the complexity of ensuring access to care, providing optimal staffing, and continuing to train resident physicians. To address this complex coordination, most hospitals created excel or other flat-file (analogous to paper-based) tracking systems, requiring manual input and update. Without a centralized system, accessing and generating readiness assessments is time-intensive and error-prone. Additionally, there is no manpower-allocation to complete this required coordination, resulting in additional duties for already-taxed MTF personnel.
With subsequent assignment changes, and without formal MTF input into the assignments process, MTOE units select the physicians to fill the assignments using the Assignment Interactive Module Version 2 (AIM2). For most non-medical MTOE units, multiple specialties may fill a given position, with AR 601-142 listing the suitability criteria. As an example, 20 different specialties may fill a 62B, field surgeon, position. Usually, a 60P pediatrician, 61F internist, or 61H family physician fills this position.
The general nature of this position increases the complexity of talent management, as non-matched specialty replacements, such as an internist replacing a family physician, may have significant impacts when the incumbent fills an important MTF role, such as residency faculty. This would potentially remove residency faculty or other departmental leadership positions across assignment cycles. Limitations in the personnel inventory preclude the full exclusion of key personnel from the MAP process. As a result, a faculty or department chair may have primary duties outside the MTF, dividing work priorities and decreasing effectiveness and availability.
Validation
Organizational change is a constant within the Army, due to assignment cycles, shifts in priorities, and the availability of resources. Within this change, the requirement to meet the needs of combatant commanders and the national defense strategy is constant. Human capital is a limited resource, and increased systems integration provides optimized use and future adjustment. Further, ensuring quality through management of clinical employment is critical to preserving the medical readiness of the force and providing a ready medical force to meet ongoing threats. Providing an enduring solution requires integration with existing systems. The DOD acquisitions process enables this integration.
Department of Defense Acquisitions Process
The DOD acquisitions process is as complex as the briefly described Army organization and policy. As there is no current validation of the UON, I focus the background discussion on this step, with a very brief overview of subsequent steps. Multiple regulations govern the acquisitions process, with DOD Directive 5000.01 establishing authority and overarching requirements.
DOD Instruction 5000.02 describes the process for urgent capability acquisition, and helps to define the UON as DOD component-specific, given the scope limitation within the Army. To qualify as a UON, the acquisition program must field in less than two years with expected costs less than $40 million in any single fiscal year or $520 million over the lifecycle. The designation as a component-specific UON reduces the validation, program execution, and designation of the milestone decision authority (MDA) to the component level, rather than the Under Secretary of Defense level. The MDA has overall responsibility for the program and approves entry of the program into each subsequent phase.
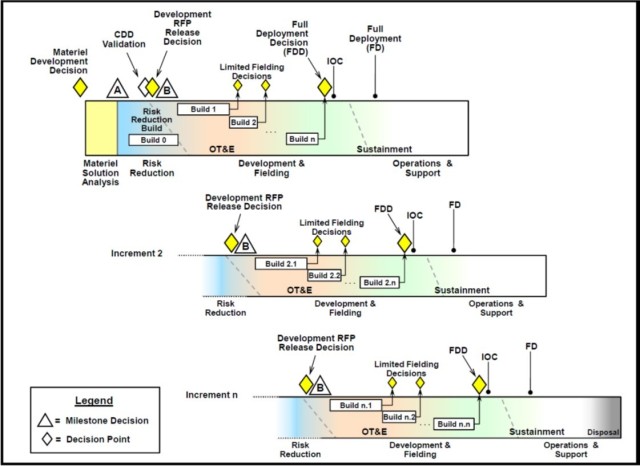
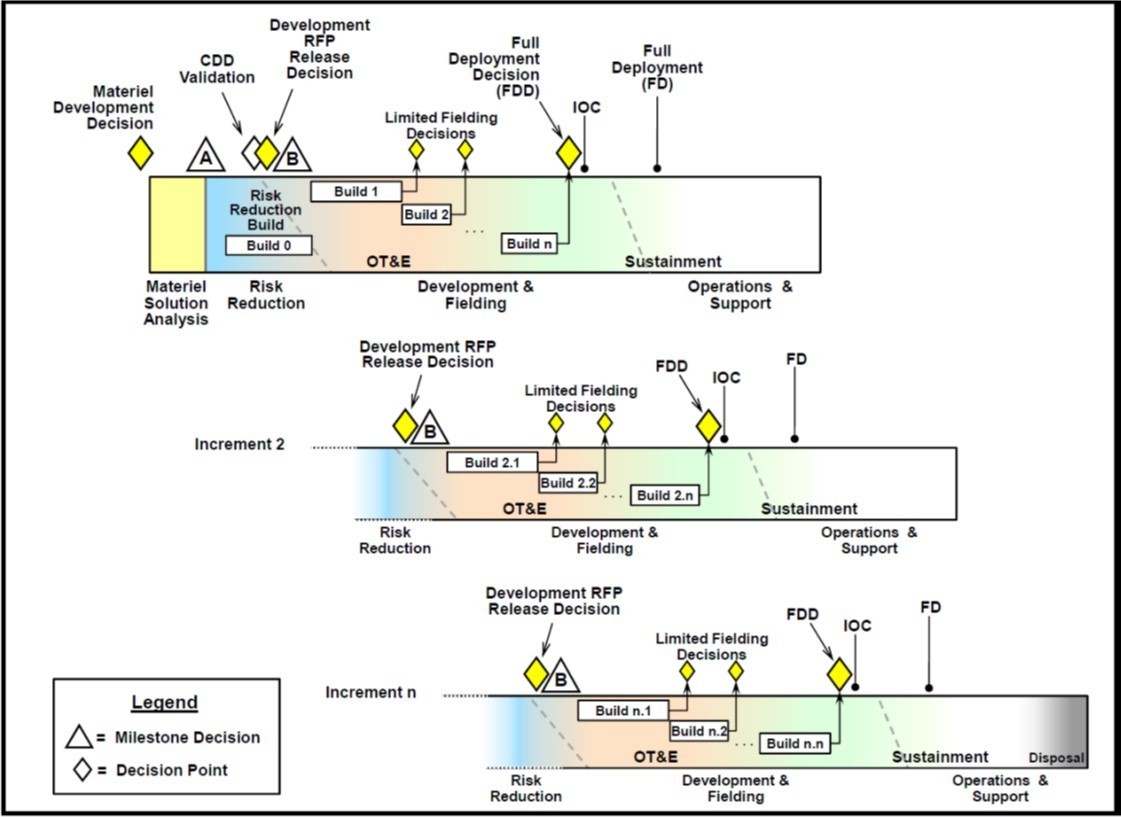
DODI 5000.02 provides graphical models of acquisitions programs with the milestone decisions designating phase transitions. The possible program models applicable to this UON are Model 2, Defense Unique Software Intensive Program, and Model 3, Incrementally Deployed Software Intensive Program. Meeting the multiple capabilities discussed further in the Connected Systems section, the most appropriate model to meet this UON is Model 3, demonstrated in Figure 1. DODI 5000.02 further defines Milestones A, B, and C. Programs progress through these milestones towards full implementation. At completion, the designed solution meets the needs of all stakeholders, in this case, providing an integrated and sustainable method for clinical quality management through analysis of availability and readiness along with talent management, ensuring the right person, in the right place, at the right time.
Stakeholders
The primary stakeholders representing Army equities are MEDCOM and Forces Command (FORSCOM). MEDCOM, commanded by the Army Surgeon General, currently retains ultimate privileging authority for all Army clinicians as well as the responsibility to advise the Army Chief of Staff regarding both the readiness status of medical personnel as well as the overall health of the Army. FORSCOM is the largest Army command, with the majority of MTOE units, representing approximately 750,000 personnel in Army components (COMPO) 1, 2, and 3: Active Army, National Guard, and the Army Reserves. Other Army commands, such as Army Pacific Command and Special Operations Command have medical officers affected, though FORSCOM is the primary representative of the common interests.
The DHA benefits from enhanced visibility providing improved clinical quality management, given the organizational responsibility for the administration of the MTFs. Additionally, DHA maintains the EHR and is the proponent for system access.
Connected Systems
Table 1 lists the systems of interest, introduced above. To meet the UON, the solution must provide a continuous and objective assessment of individual and institutional performance. System development should focus on integrating the disparate data elements from Table 1. As each system is a SOR, with a primary function, complete integration is unrealistic. Creating a dashboard, supported by a relational database with minimal two-way communication achieves this solution in concept.
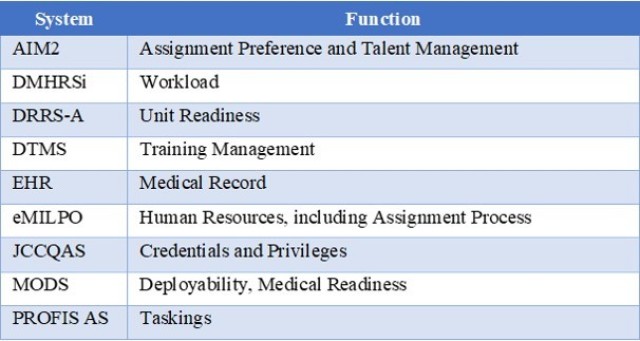
Figure 2 presents a graphical depiction of this system.
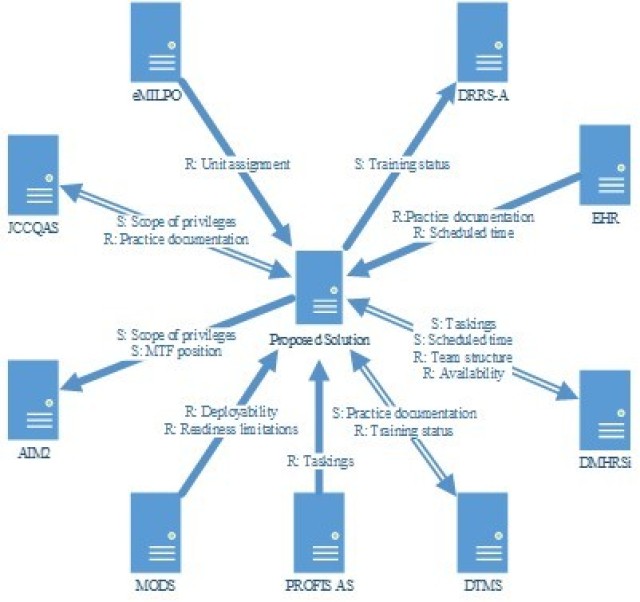
Functionally, the proposed solution receives inputs from the following systems: DMHRSi, DTMS, EHR, eMILPO, JCCQAS, MODS, and PROFIS AS. DMHRSi provides team structure and availability, both of which aid in calculating workload and planning for team staffing. Training status, sent by DTMS, along with practice documentation and scheduled time from the EHR inform analysis of AOC-specific requirements for procedures and number of patients. Current unit assignment information from eMILPO, along with the scope of privileges from JCCQAS and the practice documentation from the EHR allows individual clinical quality assessments. Analysis of deployability and readiness limitations from MODS against taskings from PROFIS AS further inform workload planning.
The proposed solution provides inputs into AIM2, DMHRSi, DRRS-A, DTMS, and JCCQAS. Primary input of MTF position allows complete tracking of positions and skills within AIM2. The individual clinical quality management assessments also inform AIM2, facilitating increased fidelity in matching skills with position requirements. Taskings from PROFIS AS and clinic schedules from the EHR aid in accurate time capture within DMHRSi, providing increased data quality compared with manual reporting. Individual training and readiness levels, assessed from multiple sources, provide data to DRRS-A based on unit assignment. These training levels also assist in the automated update of DTMS, specifically with regards to tracking practice documentation elements, such as the number of chest tubes placed for 62A Emergency Physicians. Practice patterns also inform JCCQAS to ensure the adequacy of credential maintenance and aid in increasing competency through supervised progression.
Conclusion
There is an UON for improved visibility and management of medical personnel readiness. Previously mitigated by direct control, the decentralization of management from an MTF to MTOE units clearly requires action to meet operational needs. The complexity inherent in the Army’s medical personnel management and readiness programs can benefit from increased integration. Once validation of UON occurs, the DOD acquisitions process enables further action. Providing an integrating solution for multiple SOR can meet this need and provide further automation and functional integration.
--------------------
Lt. Col. Barrett H. Campbell, MD, MBA, PMP, CPE, FAAFP is a family physician and current fellow, Clinical Informatics at Madigan Army Medical Center in Tacoma, Washington. He graduated from the United States Military Academy at West Point in 2005 with a Bachelor of Science, majoring in Life Science with a Computer Science engineering track. He graduated with his M.D. from the Uniformed Services University in Bethesda, Maryland, in 2009. While at USU and in conjunction with the Office of Student Affairs, Campbell developed and maintained a web-based Clerkship Management Program used by the University over the following decade to provide selection and management of Clerkship rotations for medical students. Dr. Campbell completed Intermediate Level Education at the Command and General Staff College in Fort Leavenworth, Kansas, also earning his MBA from Webster University, in 2017. He is currently completing his Master of Health and Clinical Informatics at the Oregon Health & Science University.
--------------------
This content is published online in conjunction with the April-June 2021 issue of Army Sustainment.
RELATED LINKS
The Current issue of Army Sustainment in pdf format
Current Army Sustainment Online Articles



Social Sharing