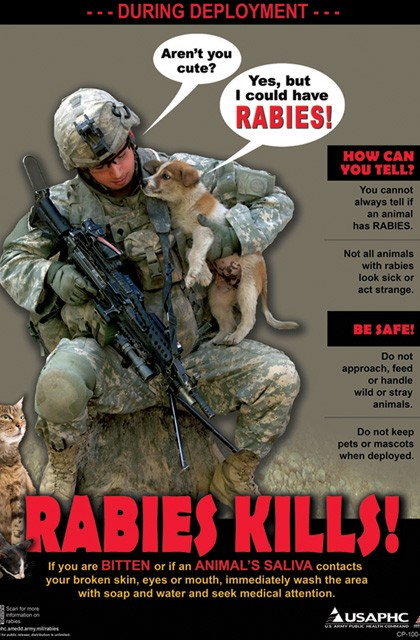
FORT RUCKER, Ala. (Mar. 22, 2012) -- Soldiers preparing for deployment have many things to be aware of, but there is one potential danger many may not have considered -- the danger of rabies.
"It's a big deal. It's out there," said Capt. Tiffany Flowers with the Fort Rucker Animal Treatment Facility. "People don't think about it because our animals are regularly vaccinated for rabies, but over there, they're not. That's the lowest thing on the list of things to think about."
After a Soldier died from rabies last year, troops across the military were asked to be more aware of the risk and to report any previously unreported contact with potentially infected animals.
Here at Fort Rucker, the instructions are more specific. Any Soldier who had contact, such as a bite or scratch, with a potentially infected animal while on deployment since Sept. 1 and did not report it is asked to report it now. Also, any Soldier who reported contact and has not received treatment for rabies is asked to report that as well, said Maj. Laura E. Ricardo, chief of preventative medicine at Lyster Army Health Clinic.
"It's a deadly disease and it's completely preventable. But if it goes unreported and untreated, it can lead to death," said Ricardo.
Rabies in humans is 100 percent preventable through prompt appropriate medical care, according the Centers for Disease Control and Prevention website at http://www.cdc.gov, advising that it's important to remember that rabies is a medical urgency; decisions should not be delayed.
One of the most effective ways to decrease the chance for infection is to wash the wound thoroughly with soap and water, the CDC further advises.
Flowers admits it can be difficult to know when to report contact because an animal can carry rabies for up to six months before symptoms appear. During this time, the animal can still infect others.
"It's a tough spot. The stray population is really bad. When you go off a forward operating base, you've got all these strays running around and somebody's carrying rabies. Somebody's got it," she said. "The actual symptoms are neurologic-type signs such as behavioral changes, definite aggression, and, of course, salivating … just think about the end of Old Yeller."
The first symptoms of rabies may be very similar to those of the flu, including general weakness or discomfort, fever or headache. These symptoms may last for days, according to the CDC. There may be also discomfort or a prickling or itching sensation at the site of bite, progressing within days to symptoms of cerebral dysfunction, anxiety, confusion, agitation. As the disease progresses, the person may experience delirium, abnormal behavior, hallucinations and insomnia.
The acute period of disease typically ends after two to 10 days. Once clinical signs of rabies appear, the disease is nearly always fatal, and treatment is typically supportive, according to the CDC. To date less than 10 documented cases of human survival from clinical rabies have been reported and only two have not had a history of pre- or postexposure prophylaxis, according to the CDC.
Disease prevention includes administration of both passive antibody, through an injection of human immune globulin and a round of injections with rabies vaccine.
"Most people first develop symptoms of pain, tingling, itching or a shooting sensation originating from the bite site," Ricardo said, adding that other symptoms can appear similar to the flu, so it is important for doctors to know about any potential exposure to rabies when treating a patient.
"I want to emphasize that it's not too late. I don't want someone to say they were bitten back in September so it's too late or it must be gone," she added. "It's worth it all for one life."
All reports of contact with potentially infected animals should be directed to Ricardo at 255-7376.

Social Sharing