Most of us have had that “uh-oh” feeling usually accompanied by the desperate urge to find the “head” or “latrine” ASAP. This thought might be followed by, “Did I get some kind of stomach bug?”
Acute gastroenteritis illness, or AGI, commonly referred to as a “stomach bug,” can spread quickly through communities. It typically causes symptoms such as diarrhea, stomach pain or cramping, nausea, vomiting and sometimes fever and fatigue. Dehydration is a serious concern, especially in young children and older adults. Symptoms may last a day to over a week depending on the type of infection.
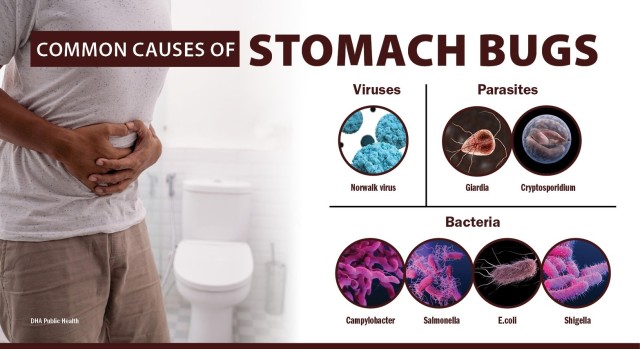
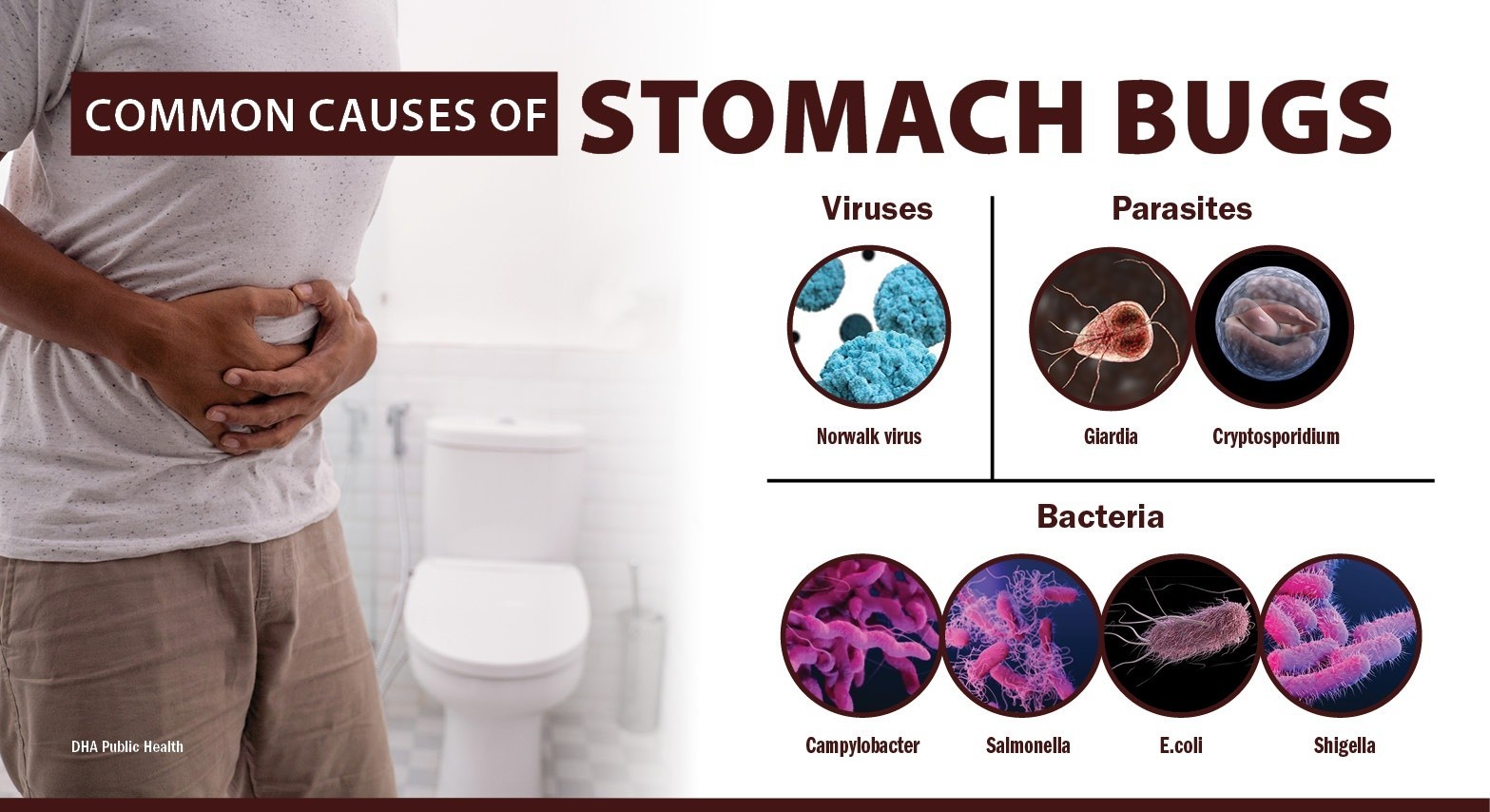
An AGI is often caused by a virus, bacteria, or parasite that has been unknowingly ingested, usually from a contaminated food or water source. These infections can lead to intense symptoms, including both vomiting and diarrhea, commonly described as “coming out both ends.”
Though AGIs occur year-round, they are often associated with food- and water-borne germs during the summer months, according to Defense Health Agency–Public Health experts.
“The cause may be traced to one’s own backyard, a local food source, or recreational activity,” said Dr. Charles McCannon, a medical doctor working for the preventive medicine division of the DHA-PH at Aberdeen, Maryland. “While the specific type of bug or germ responsible for the illness may not be identified, both the symptoms and the way to minimize the risk of getting sick are often the same.”
AGIs Are No Joke
“Most of the time, AGIs get better without treatment, but in certain people with weakened immune systems, the illness can become severe enough to require hospitalization or even cause death,” said McCannon.
Even in healthy adults, an AGI can impair a person’s ability to work and perform physical tasks, said McCannon. It can take days before symptoms improve, and a patient often needs time to rest for full recovery. Additionally, the dehydration and diarrhea associated with AGIs can also increase the risk of heat illness in hot environments.
The Military Is Not Immune
AGIs have long been a significant cause of illness among U.S. service members, said McCannon.
“In fact, U.S. service members have been found to be less likely to seek medical treatment than civilians,” he said. “By choosing to ‘tough it out’ while sick, service members are likely not going to be operating at their best and may increase the spread of germs to others in their units.”
AGI outbreaks in the military have resulted in temporary suspension of training, quarantining to barracks, efforts to disinfect barracks floors, and increased inspections of military eating establishments, said McCannon.
To identify possible outbreaks before they can affect military readiness, DHA-PH experts routinely monitor medical visits for several common AGI diseases. The diseases, categorized as reportable medical events, or RMEs, are required to be documented by military hospitals and clinics across all services in what’s called the DHA Disease Reporting System internet or DRSi.
To know the actual disease name, a patient must seek medical evaluation that includes laboratory testing to identify the specific type of virus, bacteria, or parasite. The diseases identified are reported in the Medical Surveillance Monthly Report, known as the MSMR. However, since many cases of AGI are not diagnosed with the specific diseases, the number of reported cases is much lower than the number of service members infected.
“Most of the AGIs have similar symptoms and most people ‘self-treat,’ meaning service members don’t seek medical treatment,” said McCannon. “So, we know the reported medical data are just the tip of the iceberg. The actual impact to military readiness is even larger than what is suggested by the numbers of cases.”
Understanding Food- and Water-Borne Diseases of Military Concern
The most frequently diagnosed food- and water-borne AGI disease is Norovirus, also referred to as the Norwalk virus. In 2024, the next five most common AGI diseases in the military included campylobacteriosis, salmonellosis, giardiasis, E.coli infection, cryptosporidiosis, and shigellosis. Each year, thousands of service members seek medical treatment and are diagnosed with these diseases.
Most food- and water-borne diseases of military concern have similar symptoms and types of sources, said McCannon. In general, the germs that cause these diseases may last hours to days on surfaces and may live weeks, months or even years in some environments. Variations include time of symptom onset and duration of symptoms. Most patients are treated for the symptoms, though antibiotics may also be prescribed for some.
McCannon explains that these common diseases occur everywhere and are consistent with occurrences in the civilian population. Service members can be at higher risk of exposure when performing duties in field, operational, or other austere conditions. Less common diseases, like amebiasis and hepatitis A or, more rarely, botulism, cholera, Listeriosis, and typhoid fever, are often associated with exposures overseas.
“It might sound gross, but most of the viruses and bacteria transmitted in food and water sources initially come from fecal matter of an infected animal or human,” said McCannon. “Until a body’s immune system can fight them off, the germs often live and multiply in the gut. Then the infectious germs are excreted, especially in diarrhea and vomit.”
McCannon said diseases are spread when the microscopic infectious germs get into drinking water, meat or seafood products, onto fruits or vegetables, or on surfaces that have been contaminated by infectious food products. A patient may ingest the germs directly from a food or water source. Sometimes they are infected by touching their mouth after contact with a contaminated object.
While AGIs are not spread through the air, they can be passed from a sick person to other people by activity such as not washing hands properly after using the bathroom, or by touching doorknobs, phones, or utensils. This is why these diseases are considered infectious or communicable.
“As an example, Norwalk virus is considered a very contagious disease because the virus can easily be spread from a sick person to other people when they get virus particles on their hands from surfaces or items,” said McCannon. “The virus can survive 12 hours on hard surfaces. People who contact the contaminated surfaces of items and then touch their mouths can become sick.”
How Service Members Can Reduce Spread and Lower Risk
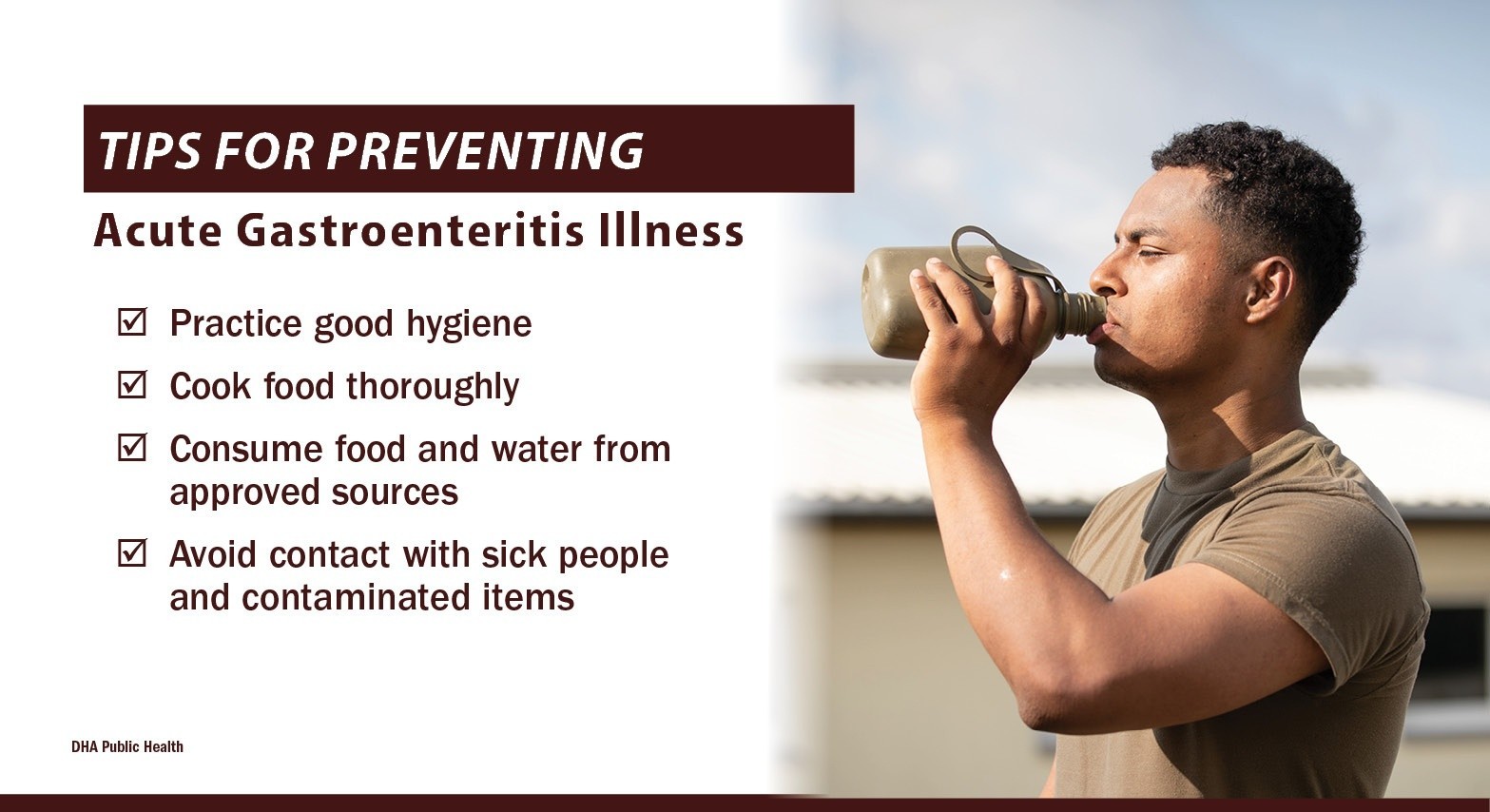
While there are no vaccines to prevent these specific diseases, they’re largely preventable by practicing good hygiene, cooking food thoroughly, consuming food and water from approved sources, and avoiding contact with contaminated sources, said McCannon.
Figure #1 (Defense Health Agency-Public Health graphic illustration by Michelle Phillips)
He offered the following tips:
- Keep your hands clean—always!
- Wash hands with soap and water for at least 20 seconds often, especially:
- After contacting food, animals, other people who may be sick (or their clothing or linens they use)
- Before and after handling or touching food or utensils/surfaces.
- Use gloves to avoid contacting potential germs.
- Clean and disinfect:
- Areas where a person or pet recently had diarrhea or vomited
- Potentially contaminated food utensils or surfaces (such as those in contact with raw meat or unwashed produce)
- Cook meats and shellfish thoroughly. In general, processed meet like hamburgers should be well-done, with no pink showing. But since meat can brown before it's completely cooked–especially in outdoor grilling–it’s best to use a meat thermometer to ensure the meat is heated to at least 160 F (71 C) at its thickest point.
- Drink pasteurized milk, juice, and cider.
- Wash fruits and vegetables.
- Wash laundry in hot water.
- Avoid swallowing water while swimming.
- Boil or filter water from lakes, springs or rivers before drinking or preparing food with it.
Help Limit the Spread
Once sick, the most important thing a service member can do is help limit the spread, said McCannon. Avoiding contact with a sick person or their belongings is important, but that isn’t always practical.
“In certain military settings, close contact and shared quarters are a recognized concern,” he said.
McCannon recommended staying at home or isolating from casual contact with others as much as possible, ideally, for two days after symptoms stop. For more intimate contact, it’s best to wait much longer, like several weeks after you or your partner has been sick with an AGI.
While sick, don’t eat or drink anything that makes diarrhea worse, like dairy products, caffeine, or alcohol, said McCannon. Drink plenty of fluids to stay hydrated. For most AGIs, treatment includes rest and fluids to help prevent dehydration and fatigue. But consider seeking medical evaluation for a specific diagnosis of diarrheal illness.
Knowing the name of the germ causing your stomach bug may not change the treatment, but knowing the diagnosis can help our military’s public health experts identify trends and address outbreaks to keep our forces strong.
Additional Resources
- Defense Health Agency - Diarrheal Food- and Water-Borne Diseases
- Defense Logistics Agency, Food Safety Office Food Safety/Recall Messages
- Navy Food Sanitation and Safety Library
- DoD Food Safety Inspections
- Food and Drug Administration: “What You Need to Know about Foodborne Illnesses”
- Causes of Foodborne Illness: FDA Bad Bug Book (Second Edition)
The Defense Health Agency supports our Nation by improving health and building readiness—making extraordinary experiences ordinary and exceptional outcomes routine.
NOTE: The mention of any non-federal entity and/or its products is for informational purposes only, and is not to be construed or interpreted, in any manner, as federal endorsement of that non-federal entity or its products.
Social Sharing