
The Heat is On: A Serious Threat
Service members routinely face real-world medical readiness challenges during deployments and the outdoor training exercises that prepare troops for combat. Heat stress is one of the most common of these environmental threats. Becoming a casualty of heat stress can reduce both individual and unit-fighting strength.
Not Just Hot Days: Understanding the Risks
Heat illness was among the top five most reported medical events among U.S. active duty service members in 2024, with cases peaking in the June through July timeframe.
While many heat casualties occur when outside temperatures climb above 75 degrees Fahrenheit, heat illnesses cases in the military primarily occur during extended rigorous outdoor activities while service members are wearing uniforms and carrying equipment. As a result, heat illnesses are reported all year, even when environmental conditions represent a low-risk military heat category.
But military experts say persistent education and increased awareness are helping catch service member heat illnesses early, which prevents the most serious conditions. This has occurred even as average outdoor temperatures have been continuing to rise for the past several years.
The reduction in severe heat illness cases has been proven by Defense Health Agency-Public Health experts at Aberdeen Proving Ground, Maryland, who monitor military cases of heat illness to inform prevention policies, doctrine, and training.
“The number of overall military heat illnesses has risen. The good news, however, is that the number of heat stroke cases, which is the most severe form of heat illness, has been decreasing,” says Alexis Maule, a senior epidemiologist at Defense Health Agency-Public Health at APG.
“This decrease in training casualties helps reduce lost training days,” says Mike Reed, chief of Research, Studies and Analysis at the U.S. Army Combat Readiness Center in Fort Novosel, Alabama.
“Risk is highest among recruits who are not yet accustomed to the level of physical activity and warm- or hot-temperature environments,” Reed says. “In addition to time and resources needed for treatment, the casualties also result in lost training and duty days, or worse.”
Reed notes that heat stress is an unavoidable hazard of military duty, but death due to heat stroke is 100% preventable.
“High-risk activities include initial training programs, foot marches, running-related exercises, and land navigation,” says Reed. “However, the increased awareness of the risks and of treatment actions appears to be allowing more cases to be caught earlier and is reducing severe cases in military training programs.”
The dedicated efforts of the military health community are increasing knowledge and awareness of the signs, symptoms, and lifesaving actions needed to prevent heat illnesses.
Recognizing the Enemy: Heat Illness Explained
“Heat illnesses include several medical conditions that have different levels of impacts,” says U.S. Army Lt. Col. David DeGroot, Director of the Army Heat Center located at Fort Benning, Georgia. “These conditions occur when the body’s internal temperature control system can’t keep up with the heat stress demands.”
Medical conditions such as dehydration, lack of electrolytes, and heat cramps are the mildest forms of heat illness. These conditions may lead to more severe conditions if the causes for example, heat stress, hydration, and nutrition with electrolyte status) are not addressed.
Heat exhaustion, a more serious level of heat illness, is a clinical condition that must be reported to the military medical surveillance known as Disease Reporting System internet, or DRSi.
Heat stroke, the most severe form of heat illness, is a medical emergency which also must be reported to DRSi. Heat stroke can result in multiple-organ shutdown and death if there is no immediate cooling with ice, and proper treatment.
“Within the military we most commonly see exertional heat stroke, or EHS, as opposed to classic heat stroke, which is typically seen in the elderly during heat waves, or in young children. Exertional heat stroke is different because in addition to experiencing heat and humidity, the body is producing a lot of heat during physical work,” says DeGroot.
One of the most vulnerable organs is the brain. Brain dysfunction can lead to confusion, disorientation, seizures, and even coma.
“Though a hallmark of EHS is a core body temperature of 104 F, core temperature is generally not known in the field. So, we train personnel to be aware of signs that the brain is being affected, such as disorientation, slurred speech, combativeness or even loss of consciousness,” says DeGroot.
DeGroot’s recent work has shown the critical importance of immediately using the military’s field-expedient ice sheet cooling method (bed linens soaked in ice water) to treat a suspected heat-stroke casualty.
”Rapid body cooling in an ice bath has been shown to work at athletic events, but that technique is not practical in military field environments. We now have evidence that immediately cooling a heat-stroke casualty by wrapping their body in ice sheets in the field before transporting for further medical treatment can save a life,” he says.
Those at Greatest Risk: Keeping Our Forces Safe
DHA-PH data show that soldiers and Marines have had the highest rates of heat exhaustion and heat stroke among the services, and cases among younger male recruits are the most frequently reported, especially for EHS cases.
“It is unclear if there is a sex-based difference in risk, but some data suggest female service members may be less susceptible to organ damage from EHS than their male counterparts,” says Dr. Gabrielle Giersch, a physiologist at the U.S. Army Research Institute of Environmental Medicine. “The findings show female service members with EHS spent approximately half as much time in the hospital following admittance compared with the men.”
DeGroot explains some additional factors that can increase a service member’s risk:
- Weather (temperature, humidity, wind). Though military cases are reported most frequently during the warmer months of May through September, heat-related casualties have occurred in just 70 F weather. Locations such as Fort Benning, Georgia, and Fort Bragg, North Carolina, typically have the highest reported heat illness cases in the military due to their training missions, warm temperatures and high humidity.
- Strenuous physical activities. The body creates internal heat during exercise. In addition to road marches and training exercises, physical training tests, and running competitions are also risky events.
- Clothing and equipment. Service members wear full uniforms and carry heavy gear which can restrict heat loss. Specialized gear such as armor or chemical protective clothing can further add to the body’s heat stress.
- Inadequate hydration. A combination of a person’s thirst level, body weight, and urine color may help determine if a person is at risk of dehydration. Drinking fluids (water) and eating adequate foods can help ensure hydration and electrolytes.
- High motivation to excel. Data show higher than expected heat-illness casualties among military personnel in training schools. This is likely because trainees are competitive and exert themselves beyond their physical limits to complete tasks.
Frontline Defense: What Can Service Members Do?
“While the military can’t avoid hot environments, we can control how we prepare for and handle them,” says DeGroot. “Heat illness is preventable, and knowing the right steps can save lives—including your own.”
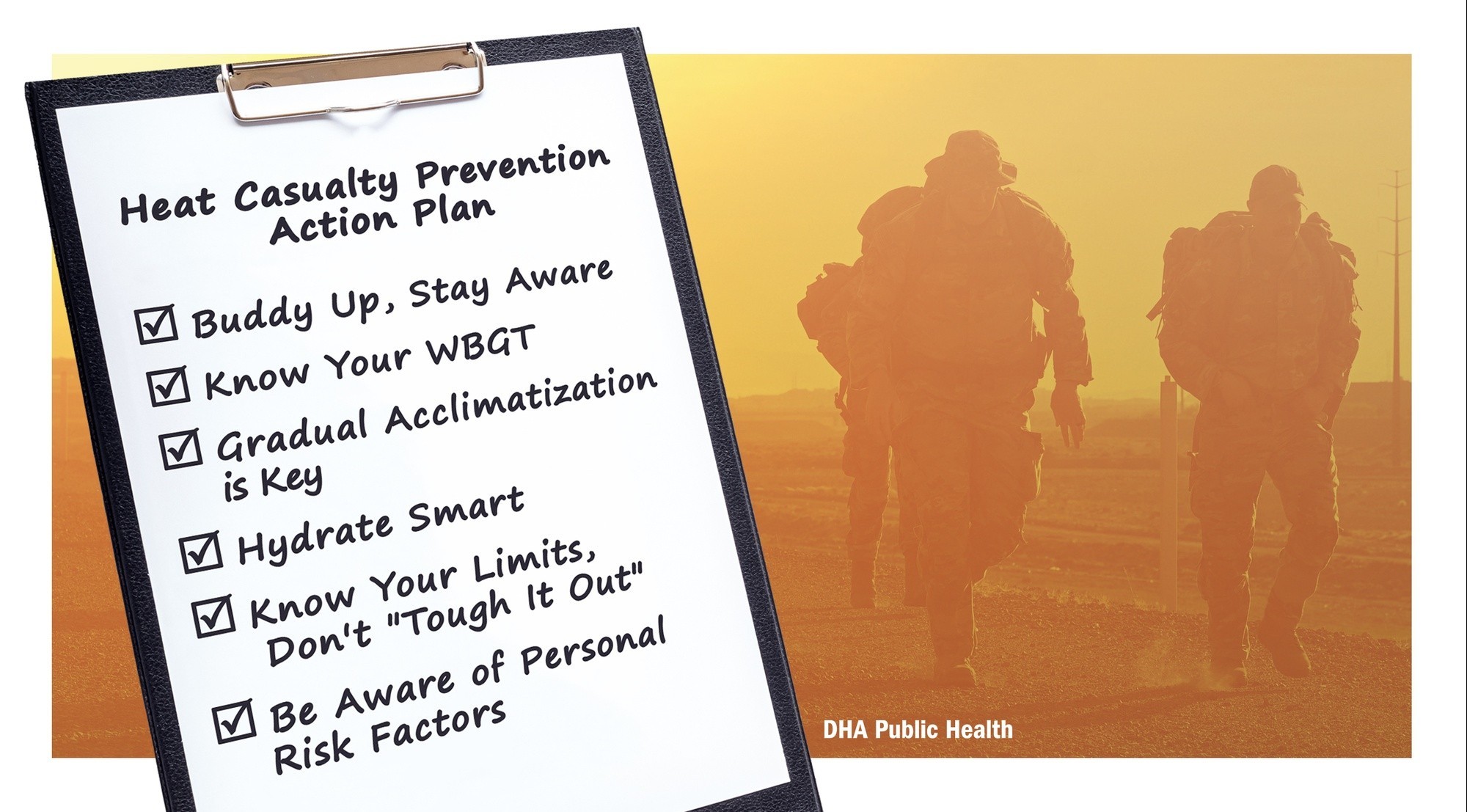
Here’s Your Action Plan:
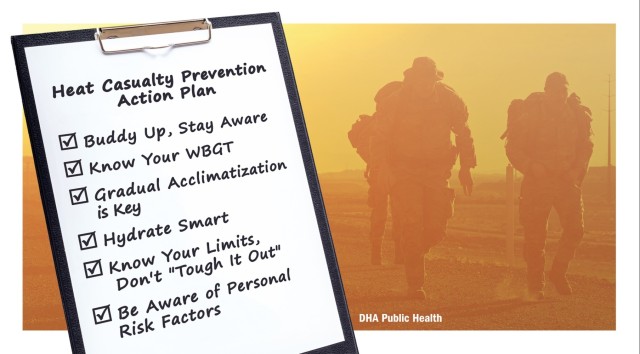
- Buddy Up, Stay Aware: Watch out for each other! Monitor hydration levels and look for early signs of heat illness. If something seems off, speak up.
- Know Your WBGT: The Wet Bulb Globe Temperature, known as WBGT, tells you more than just the air temperature. It factors in humidity, wind, and sun exposure to give you a better picture of heat-stress risk.
- Factor in Your Gear: Add 5 F to the WBGT if you're wearing a rucksack or body armor, and 10 F for full chemical protective gear.
- Adjust for Safety: Avoid WBGT Risk Categories 4 and 5, especially on consecutive days. Plan activities for cooler times: night, before sunrise, or in the shade. Factor in previous days’ WBGT levels—multiple hot days increase your risk.
- Gradual Acclimatization is Key: Give your body time to adjust to both hot climates and high-exertion levels. This takes one to two weeks—start increasing activity before moving somewhere warmer.
- Hydrate Smart: Follow military work/rest and water consumption guidelines.
- Don't exceed fluid intake limits: 1 quart of water per hour, or 1.5 quarts during intense activity. Overhydration can be dangerous by diluting the chemical balance of the body.
- Track your intake: Use knots on your gear or another visual method to show how much water you've consumed. This also helps medics if you experience heat illness.
Know Your Limits, Don’t “Tough It Out”:
- Recognize the early signs of heat illness.
- If you’re feeling the effects of heat, tell someone. Pushing through it can have serious consequences.
Be Aware of Personal Risk Factors: Certain factors can make you more susceptible to heat illness. Inform your buddy and medical staff about:
- Previous heat illness
- High body mass index, or BMI
- Current illness or any relevant health conditions
- Recent alcohol consumption
- Certain medications (antihistamines, blood pressure meds, decongestants, antidepressants, some diuretics)
Additional Tips: Even when performing military duties, always consider ways you might be able to reduce the risk on your body:
- Lighten loads and modify clothing to increase air circulation.
- Move to the shade.
- Take frequent rest breaks.
Remember:
“Every heat illness death is one too many,” says DeGroot. “By being proactive and looking out for ourselves and each other, we can minimize risks and complete our missions safely.”
Learn more:
- DHA Heat Illness Web Resource
- Military Health Illness Prevention Brochure (2023)
- Military Heat Illness Prevention and Treatment Videos
- New military technology to prevent heat stroke (2024)
- Military Doctrine: Technical Bulletin 507, HEAT STRESS CONTROL AND HEAT CASUALTY MANAGEMENT (2022)
The Defense Health Agency supports our Nation by improving health and building readiness–making extraordinary experiences ordinary and exceptional outcomes routine.
NOTE: The mention of any non-federal entity and/or its products is for informational purposes only, and is not to be construed or interpreted, in any manner, as federal endorsement of that non-federal entity or its products.

Social Sharing