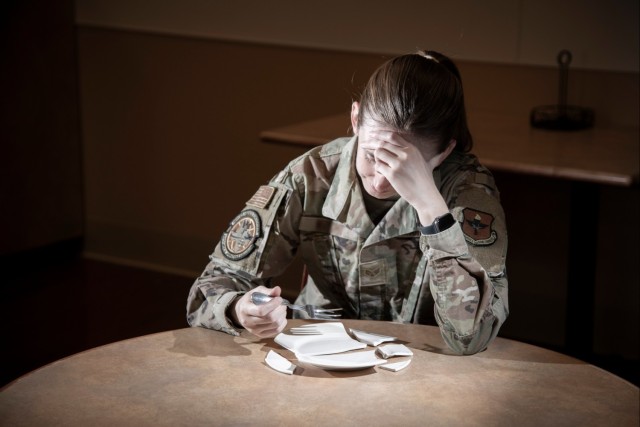
JOINT BASE SAN ANTONIO-FORT SAM HOUSTON, Texas, Feb. 28, 2024 – According to recent articles in the International Journal of Eating Disorders, children of U.S. military members may be at increased risk for eating disorders.
Data indicated that military children and adolescents experience significantly more eating disorder symptoms compared to their civilian peers. Nearly a quarter of adolescent female dependents screen above clinical cut-offs for significant eating disorder symptoms, about three times the rate in civilian populations.
“Our Adolescent and Young Adult Clinic sees patients with eating disorders regularly,” said Air Force Lt. Col. (Dr.) Michelle Lawson, Adolescent Medicine physician. “Our military population – active duty and dependents – are not immune to eating disorders and arguably, our fitness culture may promote the development of eating disorders.”
Lawson encourages families to bring up concerns if they notice any changes in eating behaviors or negative image-related mentality including skipping meals, secretive eating, fixation on certain types of foods, food rules, distorted body image, significant increases in exercise related activities or purging.
“Changes in eating behaviors may or may not correlate with changes in weight or appearance but often can start to affect mood,” Lawson said. “Increased irritability and emotional lability, difficulties with concentration or increasing fatigue along with changes in eating behaviors are concerning and warrant further evaluation.”
“It is vitally important to recognize that eating disorders can affect all ages, races, ethnicities, genders and social/economic status,” she added. “Eating disorders are also present across all shapes and body sizes.”
According to the National Institute of Mental Health, the most common eating disorders are anorexia nervosa, bulimia nervosa, binge eating, and avoidant/restrictive food intake disorder.
Anorexia nervosa is a condition where people avoid food, severely restrict food, or eat very small quantities of only certain foods. They also may weigh themselves repeatedly. Even when dangerously underweight, they may see themselves as overweight.
Bulimia nervosa is a condition where people have recurrent and frequent episodes of eating unusually large amounts of food and feeling a lack of control over these episodes. This binge-eating is followed by behavior that compensates for the overeating such as forced vomiting, excessive use of laxatives or diuretics, fasting, excessive exercise, or a combination of these behaviors.
Binge-eating disorder is a condition where people lose control over their eating and have reoccurring episodes of eating unusually large amounts of food. Unlike bulimia nervosa, periods of binge-eating are not followed by purging, excessive exercise, or fasting. Binge-eating disorder is the most common eating disorder in the U.S.
ARFID, also known as selective eating disorder, is a condition where people limit the amount or type of food eaten. Unlike anorexia nervosa, people with ARFID do not have a distorted body image or extreme fear of gaining weight. ARFID is most common in middle childhood and usually has an earlier onset than other eating disorders. Many children go through phases of picky eating, but a child with ARFID does not eat enough calories to grow and develop properly, and an adult with ARFID does not eat enough calories to maintain basic body function.
“Most subject matter experts would still agree that the adolescent and young adult population has the highest incidence, or new diagnosis, of eating disorders,” Lawson said. “However, there is concern that the incidence of eating disorders in children younger than age 12 is increasing in developed countries including the United States.”
Overall, the goal is to create home, school and work environments that foster well-being, such as supporting building self-esteem, body acceptance, and a healthy relationship with the body, eating, and physical activity, she advised.
Some tips include:
• Avoid unhelpful words describing body appearance such as fat, big-boned or other potentially triggering words unique to each patient.
• Similarly, aim to create a non-diet culture with minimal to no comments or discussions about dieting.
• Avoid calorie counting, frequent weight checking at home. Instead, focus on balanced, regular meals in a supportive environment.
• Encourage opportunities to engage in physical activity in non-weight focused/safe environments.
• Avoid unhelpful food labelling (‘good’ or ‘bad’) as this labeling may then be associated with guilt and frustration. Instead, encourage intuitive eating practices with increased awareness of hunger cues and control of mood and subsequent eating behaviors.
• Reach out to healthcare professionals for further recommendations based on unique, individual circumstances.
“Depending on the severity of the eating disorder, full remission can take anywhere from 1-20 years,” Lawson said. “Healthcare professionals are encouraged to regularly screen patients for eating disorders along with mood and behavioral health concerns.”
“We are fortunate at BAMC to have professional resources available for patients who have eating disorders,” she said. “Our Departments of Pediatric and Adolescent Medicine, Behavioral Health/Psychiatry and Nutritional Medicine regularly care for active duty and dependent patients, often in partnership with each other and with local civilian programs.”

Social Sharing