Durin
g a forum at Redstone Arsenal to bring awareness of the dangerous drugs that are impacting the community, an official with the local ambulance service said it is responding to more fentanyl and opioid-related overdoses.
“We are seeing an increase in pre-hospital overdoses,” Don Webster, the community relations officer at Huntsville Emergency Medical Services Inc., said.
HEMSI responded to 909 overdoses from fentanyl and opioid-type drugs in 2022, with most of those patients transported to the hospital, Webster said. That number represents about 75 overdoses a month, or 2.5 patients per day.
Through June of this year, HEMSI has responded to 486 overdoses, at 81 a month and 2.7 overdoses a day.
“The numbers have gone up this year,” Webster said. “That is alarming.”
HEMSI covers a growing population in Madison County, including the cities of Huntsville and Madison, and the Huntsville-annexed areas of Morgan and Limestone counties.
In 2021, during the COVID-19 pandemic, “we actually saw a little dip,” in overdose numbers, said Webster, who’s been an emergency medical technician and paramedic.
“There’s a strong chance, if we can get to (an opioid overdose patient) in a short enough period of time,” that an overdose can be reversed by administering naloxone, Webster said. Naloxone is also known by the brand name Narcan.
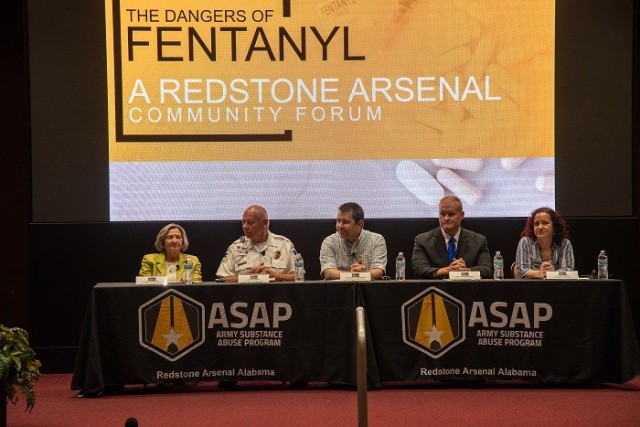
The forum, hosted by the Redstone Arsenal Army Substance Abuse Program, was held Sept. 5 at Bob Jones Auditorium and on MS Teams. Other panelists were Karren Crowson, a retired pharmacist who was previously the director of pharmacy at Huntsville Hospital; Dr. Daniel Neuberger, medical director of the Huntsville Hospital Emergency Department; Madison County Coroner Dr. Tyler Berryhill; and Ryann Yanhko, the director of the Substance Use Disorder Clinical Care program at Fox Army Health Center.
“It takes just a little bit of fentanyl to get high and it takes just a little bit more to kill you,” said Crowson, who is the chair of Partnership for a Drug-free Community’s board. A graphic she used in her presentation shows that just 2 milligrams of fentanyl is a lethal dose.
It is about 100 times more potent than morphine and 30 to 50 times more potent than heroin, according to Crowson.
Another synthetic opioid, carfentanil, which is used as a tranquilizer for large animals, has “made its way into the illegal drug market as well,” Crowson said. It is 10,000 times more potent than morphine.
“Recently two new substances are increasingly being mixed with fentanyl or heroin,” she said. Those are a class of drugs called nitazenes, a synthetic opioid, and xylazine, a drug that’s used to sedate animals.
“It’s a pretty bleak picture with fentanyl,” she said.
However, Naloxone will soon be available to purchase over the counter, according to Crowson, and the Partnership for a Drug-Free Community now has fentanyl test strips and xylazine test strips available.
“About 1½ % of our ER visits are related to adverse effects or poisoning from opioids,” Neuberger said. “My last shift in the ER (Sept. 4), I saw 18 to 20 patients. I had three fentanyl overdoses on shift.
“The interesting thing about (fentanyl overdoses) compared to a lot of other drugs is that there’s not a standard patient for this,” Neuberger said. He said the three recent overdose patients included an out-of-state visitor, a jail inmate and a teenager still living with her parents.
“It’s definitely a problem and affecting our community,” he said. “Unfortunately, it seems to be getting a little worse rather than better.”
Neuberger said the Alabama Department of Public Health’s data on fentanyl-related deaths statewide shows “a pretty clear trend in the upward direction although it may be plateauing a little bit.”
The deaths by year climbed from 121 in 2018 to 835 in 2022, according to Neuberger, who said the numbers are probably a gross underestimation.
He noted another positive development in dealing with the opioid issue. A section of the Consolidated Appropriations Act of 2023 removes the federal requirement for practitioners to apply for a special waiver before prescribing buprenorphine to treat opioid use disorder.
“I would say that probably 90% of everybody in this room knows somebody that’s fought some type of addiction in the past, whether it be a family member or a friend,” said Berryhill, the county’s chief medicolegal death investigator. “It’s something that touches all walks of life.”
Referring to Webster’s report on overdoses, “every 72 hours in Madison County, somebody dies from that overdose,” Berryhill said.
“In the past six months, we have had one confirmed case” of carfentanil, he said, and “we just had one case of xylazine in the past six months.
“The reality is, day in, day out, in the past three or four years, fentanyl is the No. 1 culprit. It’s really heartbreaking to see the way it tears family apart.”
Yanhko, a licensed professional counselor, said that if an individual has a substance abuse disorder and comes to clinical care, “we will assess for level of care” to determine what types of care are needed like medical detox, residential inpatient treatment or outpatient therapy.
“Some of the things that we’re looking for is what level of care is this individual willing to participate in,” she said. “We try to match the need with the willingness to participate.”
Outpatient individual and group family sessions are among the services offered at Fox. “We work towards relapse prevention, help them identify triggers – emotions, people, places, things that trigger that urge to use,” Yanhko said. “We look at their strengths, what do they have that’s working for them that they can use.”
Crowson described fentanyl as “an excellent drug as an anesthetic in surgery and for the treatment of cancer pain.”
Fentanyl “made its way to the market” in 1968 and was used strictly for anesthesia in surgery, Crowson said. By the 1980s, other formulations, like lozenges and transdermal patches, started coming on the market, “and these were marketed for cancer pain.”
Then came off-label prescribing and, according to the DEA, 6.5 million fentanyl prescriptions were dispensed in 2015.
In the 12 months ending January 2022, 71,000 of the overdose deaths in the country were associated with fentanyl, according to Crowson.
“How did it get so bad?” she said. The three major reasons: fentanyl is easy to make, cheap to make and provides “a huge profit margin.”
Social Sharing