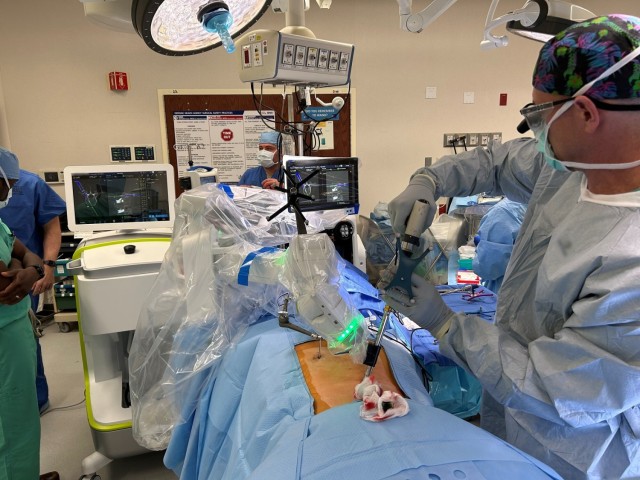
JOINT BASE SAN ANTONIO-FORT SAM HOUSTON, Texas (Jan. 25, 2023) – Brooke Army Medical Center is now using a robotic guidance system for spinal surgery that’s decreasing post-surgery pain and recovery time.
“This technology significantly improves the accuracy/precision of spinal instrumentation and is the way of the future regarding spine surgery,” said Air Force Col. (Dr.) Kenneth Bode, orthopedic spine surgeon.
The robotic guidance system allows for pre-operative or intra-operative planning, with features such as customizable implant selection, optimal implant trajectories and 3D analytics.
“The preoperative planning can be modified to patient-specific factors that are followed in the operating room exactly as planned,” Bode said. “Surgeons are able to see in three dimensions below the skin with real-time feedback of hardware placement with a single integrated picture. This novel process expands the benefits of minimally invasive surgery by combining GPS navigation and cutting-edge robotics.”
Air Force Maj. Kurt Cloutier, F-35 pilot currently serving as officer-in-charge of F-35 pilot assignments at the Air Force Personnel Center, said he’s happy that BAMC has this new technology available.
“When you see the size of the screws that they put in, you can see the margin for error is very small,” Cloutier said. “It seems like having this technology to guide the proper fit is pretty important. Two weeks post-op, I feel great. My back feels wonderful. I can imagine that if one of these screws wasn’t placed properly maybe I wouldn’t be feeling as good as I am right now.”
Bode agrees. “The patient benefits include accurate hardware placement that decreases unintentional injury to surrounding tissues to include nerves and blood vessels,” he explained. “This decreases the requirement to return to the OR (operating room) for hardware that is irritating surrounding tissues or is not stable. With less dissection and operative time, there is less pain and faster rehabilitation.”
“Since we can use navigation techniques, we do not have to remove all of the muscles from the back portion of the spine with more blood loss, operative time, and staff fatigue,” he added. “This part of the surgery is also typically quite painful causing the muscles to spasm and slows rehabilitation since they need to heal back to the bone. Now patients are able to walk the day of surgery and we have even had patients leave the hospital the same day of surgery compared with the standard postoperative course of 3-5 days.”
According to Bode, BAMC is the first in the Department of Defense to use the technology, which can benefit any patient with a spinal disorder that requires hardware for stabilization or decompression of their spine.
Patients who are contemplating spine surgery can contact their Primary Care Manager for a referral to Orthopaedic Surgery for an evaluation.
“I have personally seen the benefits of this technology and will be using this tool in as many opportunities as available,” Bode said. “Ultimately, this novel process improves and enhances our level of patient care.”
BAMC Commanding General Brig. Gen. Deydre Teyhen agrees.
“We continually strive to offer the most innovative care to our patients at BAMC,” she said. “This technology not only enables a less-invasive procedure, it also significantly reduces recovery time for our patients. I’m incredibly proud of our surgical team for their dedication to providing world-class care for our patients.”





Social Sharing