ABERDEEN PROVING GROUND, Md. – For more than a decade, military medical surveillance data analyzed by the Army Public Health Center, now Defense Centers for Public Health–Aberdeen, identified the same two leading reasons for Soldiers’ seeking medical care:
- Outpatient visits for injuries, especially overuse injuries to the bone and soft tissues of the musculoskeletal system, and
- Health encounters for behavioral health conditions that include adjustment disorders, depressive disorders, substance abuse, posttraumatic stress disorder, anxiety disorders and sleep disorders.
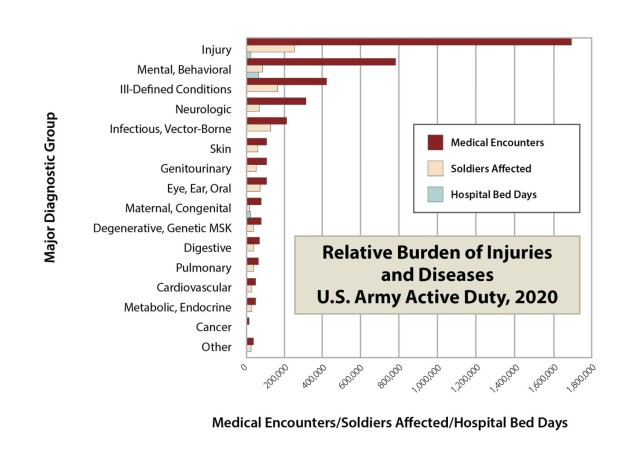
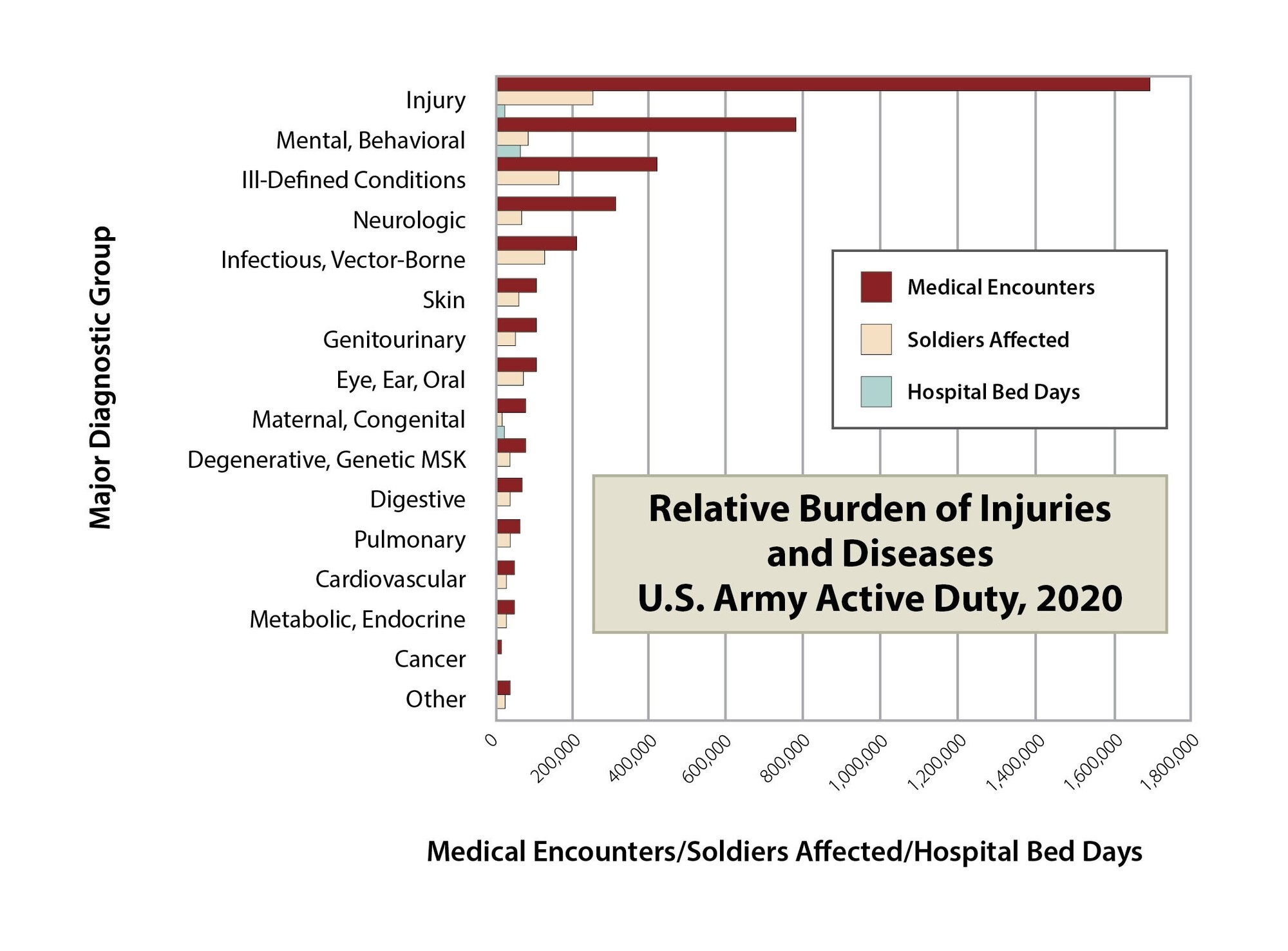
Army data repeatedly show the number of Soldiers affected by injuries and behavioral health conditions exceeds that for all other groups of medical conditions combined.
“These conditions not only require many clinical visits for treatment but also result in profiles for more days of limited duty than all other medical conditions,” says Dr. Bruce Jones, a medical doctor and retired Army colonel, now the senior injury scientist with the DCPH-A. “The temporary profiles for injuries and behavioral health conditions can affect readiness to deploy.”
Army data show approximately one out of five Soldiers may not be mission ready due to temporary medical profiles resulting from either injuries or behavioral health conditions.
The Army’s 2020 Health of the Force report, also known as the HoF, found musculoskeletal, or MSK, injuries such as overuse injuries resulted in an average of over two months of lost or limited duty time per injury. Behavioral health conditions required an average of almost three months of lost or restricted duty per Soldier receiving care.
“Reducing the severity or impact of overuse injuries and behavioral conditions on Soldiers’ health may enhance a unit’s medical readiness and fighting capability,” says Army Col. Mark Reynolds, director of the DCPH-A Clinical and Epidemiology Directorate.
Reynolds and other CPHE health experts advise commanders and leaders to optimize their unit’s health with the following tips:
TIP 1. Be a More Proactive and Engaged Leader
Leading by example and staying in touch with Soldiers is the first step toward maximizing unit strength.
According to a 2016 APHC study, less than one half of Soldiers surveyed felt leadership prioritized injury prevention and kept them informed of key injuries and risk factors. They felt many leaders were unaware of the magnitude of the adverse impacts of injury to the Army, and/or did not recognize what they as leaders can do to reduce these injuries.
According to one respondent noted in the report, “Changing the mentality of injury is a must within the military. … It starts with the drill sergeants not wanting to look weak in front of their trainees and extends up through the [Chain of Command].”
Another respondent, a medical provider, noted “Leaders … play a direct role in helping the junior Soldiers prevent and recover from injury...For example, I am treating a patient with an ankle fracture. He is in a cast and on crutches yet was made to walk for PT.”
Inconsistent leadership support or awareness has also been reported as a barrier to Soldiers seeking and continuing with behavioral healthcare. According to the DCPH-A, while behavioral health stigma has lessened over the last decade, Soldiers continue to report fears that engaging in behavioral healthcare will result in their being perceived as weak.
“It’s important for leaders to reinforce healthy habits such as good nutrition, quality sleep, adequate exercise and not misusing substances or smoking," says Reynolds. "Leaders need to motivate Soldiers to maintain their physical and behavioral or psychological health, and openly encourage use of health care resources.”
TIP 2. Know What Causes Your Unit’s Medical Non-Readiness
Individual medical readiness contributes directly to mission success. Leaders must ensure Soldiers are current on annual medical requirements, including Periodic Health Assessments, dental and eye examinations, bloodwork, and immunizations.
But being up to date on medical exams isn’t the only reason a unit is medically non-ready. Soldiers’ overuse injuries and behavioral conditions can also reduce a unit’s capabilities.
Unit leaders should be aware that these health conditions can put Soldiers out of commission for weeks. Leaders can monitor profiles and should talk to profiling healthcare providers to learn how to aid recovery and prevent recurrence.
According to Jones, some have argued that Soldiers’ medical treatments for injuries and behavioral conditions, and associated temporary profiles are the “cost of doing business.”
“But this does not have to be true,” he says. “Identification of a unit’s biggest health problems or increasing trends in a health condition can lead to meaningful modifications of training activities or enhancement of a unit’s use of local wellness resources.”
For example, the APHC data show most Soldiers’ MSK injuries include soft tissue pain and inflammation, hallmarks of overuse injuries. Overuse knee injuries, followed by the lower back, ankle and foot result in the most lost or restricted duty days. Among men, shoulder injuries also limit duty for extended periods, while hip injuries are a problem among women.
These injuries are frequently due to repetitive training activities such as running or ruck marches, says Jones. “But while these are a necessary part of military training, injury rates that are higher than average or increasing over time may indicate a unit is overtraining.”
Indicators of overtraining suggest a need to modify the training regimens. Examples of overtraining include excessive or too-rapid increases in distances, or lack of lower body recovery days between activities like running and ruck marching.
TIP 3. Monitor Your Unit’s Health and Fitness Status
Leaders are to document and monitor their unit’s fitness test results, body composition data, and profiles in the Army’s Digital Training Management System.
“If a unit’s physical fitness is decreasing over time – and injury rates are increasing – that is a cardinal sign the unit is overtraining,” says Jones.
“Each unit may have unique health conditions or risk factors that affect readiness,” says Jones. “Commanders can use the information on their unit’s health, physical fitness and training to identify existing or emerging risks to target specific hazards for prevention.”
TIP 4. Adjust Training Programs and Tactics to Optimize Physical Health
To ensure combat readiness, military policy directs commanders to maintain and enhance the physical fitness and health habits of Soldiers. For example, Field Manual (FM) 7-22, Holistic Health and Fitness, provides guidance for leaders on how to develop and maintain the physical fitness and health of Soldiers.
Basics of holistic health include ensuring healthy food and managing weight, optimizing sleep, providing for quality sleep conditions, and balancing physical training to reduce injuries.
Jones notes that employing recommended strategies that enhance physical fitness and also reduce the incidence of injuries should be among a leader’s priorities.
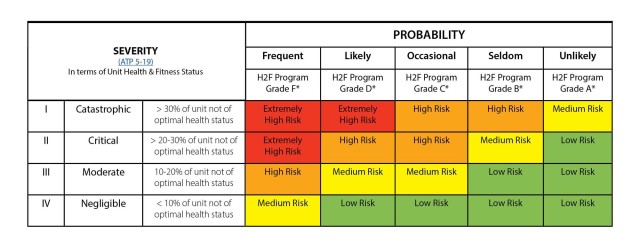
The DCPH-A offers a risk management tool adapted to reflect health and fitness policy, along with guidance that may assist unit leaders or designated staff to assess the quality and comprehensiveness of their fitness and health programs.
TIP 5. Strengthen Mental Resilience
APHC studies have found that relationship problems or family deaths, substance abuse, and sleeping difficulties are leading characteristics linked to suicides. While these life stressors may not be unique to Service members, they can be exacerbated by military life.
Leaders can help Soldiers by reminding them that the Army doesn’t expect them to be bulletproof. Leaders should encourage Soldiers to seek behavioral help just as they should use protective equipment to shield themselves from injury.
DCPH-A behavioral health experts advise leaders to be on the lookout for Soldiers who may benefit from behavioral health counseling, and to not allow harassment of those seeking help.
TIP 6. Use Your Local Experts and Reach-Back Support
Military unit strength reflects the physical and mental resiliency of individual Soldiers.
Leaders have a lot of responsibility and typically aren’t health experts; however, they have many resources at their disposal. Commanders should use data on the physical and behavioral health and fitness of their Soldiers to the extent possible to identify health and fitness problems and to make decisions about how to resolve them.
The military public health system includes medical, public health, fitness, nutrition and behavioral subject matter expertise at local, regional and Service levels.
Check with local support entities first. For information about your local installation, check out the Community Resource Guide. Installation and regional support includes –
- Local Preventive Medicine and Public Health Nurse support
- Unit Master Fitness Trainers
- Army/Armed Forces Wellness Centers (Healthy Living experts for fitness, nutrition, stress)
- Army Chaplains, Unit Ministry Teams, Unit Behavioral Health Officers, and Military and Family Life Counselors
For DCPH-A guidance regarding reducing injuries, refer to https://phc.amedd.army.mil/topics/discond/ptsaip/Pages/default.aspx for the following
- Military Injury prevention resources
- Leader’s risk matrix tool for unit health and fitness,
- Commanders Guide to Preventing MSK Injuries
- Injury Prevention Factsheets.
Recommendation regarding improvements to behavioral health problems may be found in the APHC’s Commanders Guide to Suicide Prevention.
The Defense Centers for Public Health-Aberdeen advances Joint Force health protection with agile public health enterprise solutions that supports our Nation by improving health and building readiness — making extraordinary experiences ordinary and exceptional outcomes routine.
NOTE: The mention of any non-federal entity and/or its products is for informational purposes only, and not to be construed or interpreted, in any manner, as federal endorsement of that non-federal entity or its products.

Social Sharing