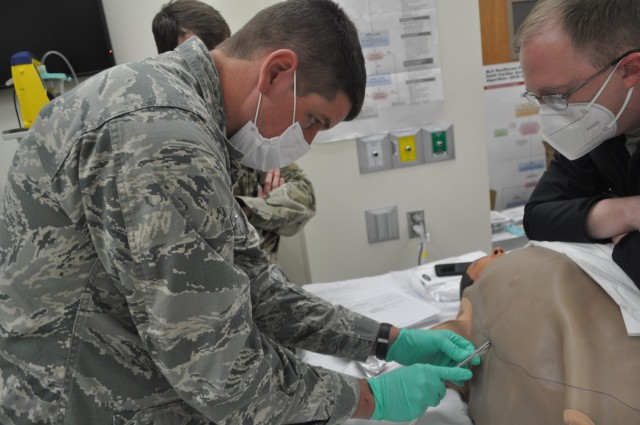
FORT BENNING, GA – “Put their arm up above their head. You can’t do this with their arm down by their side,” warned Martin Army Community Hospital Emergency Physician Capt. Jacob Arnold. “You are going to need to put a restraint on their arm or get somebody you trust to keep it down. These hurt, they suck and they [the patients] are going to move.”
Arnold walked 10 graduating residents through a chest-tube insertion as part of the Family Medicine Residency Experience (FMRx). The three-day operational medicine course is the culmination of the three-year residency program. It’s designed to teach the new doctors the Individual Critical Task Lists (ICTLs) or skills needed to treat trauma on the battlefield.
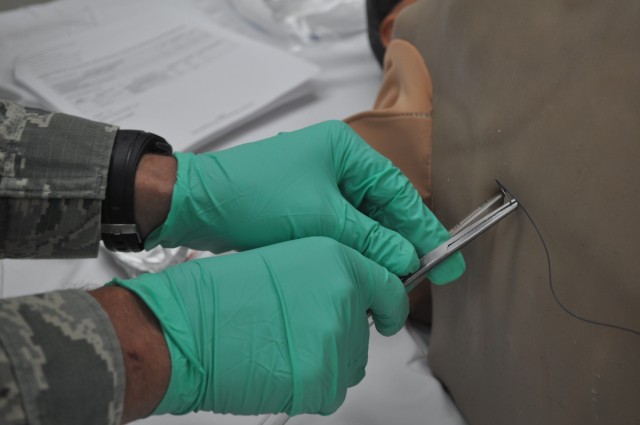
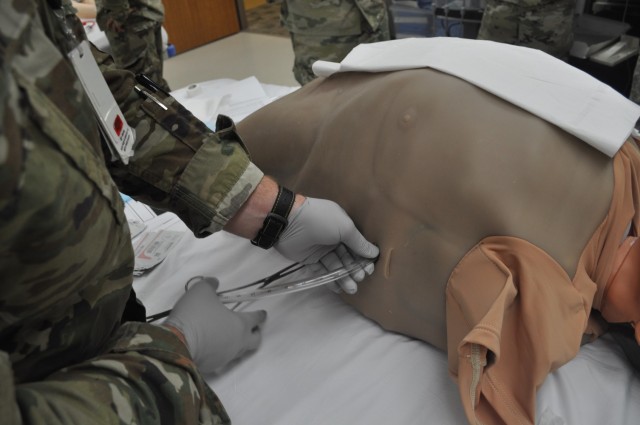
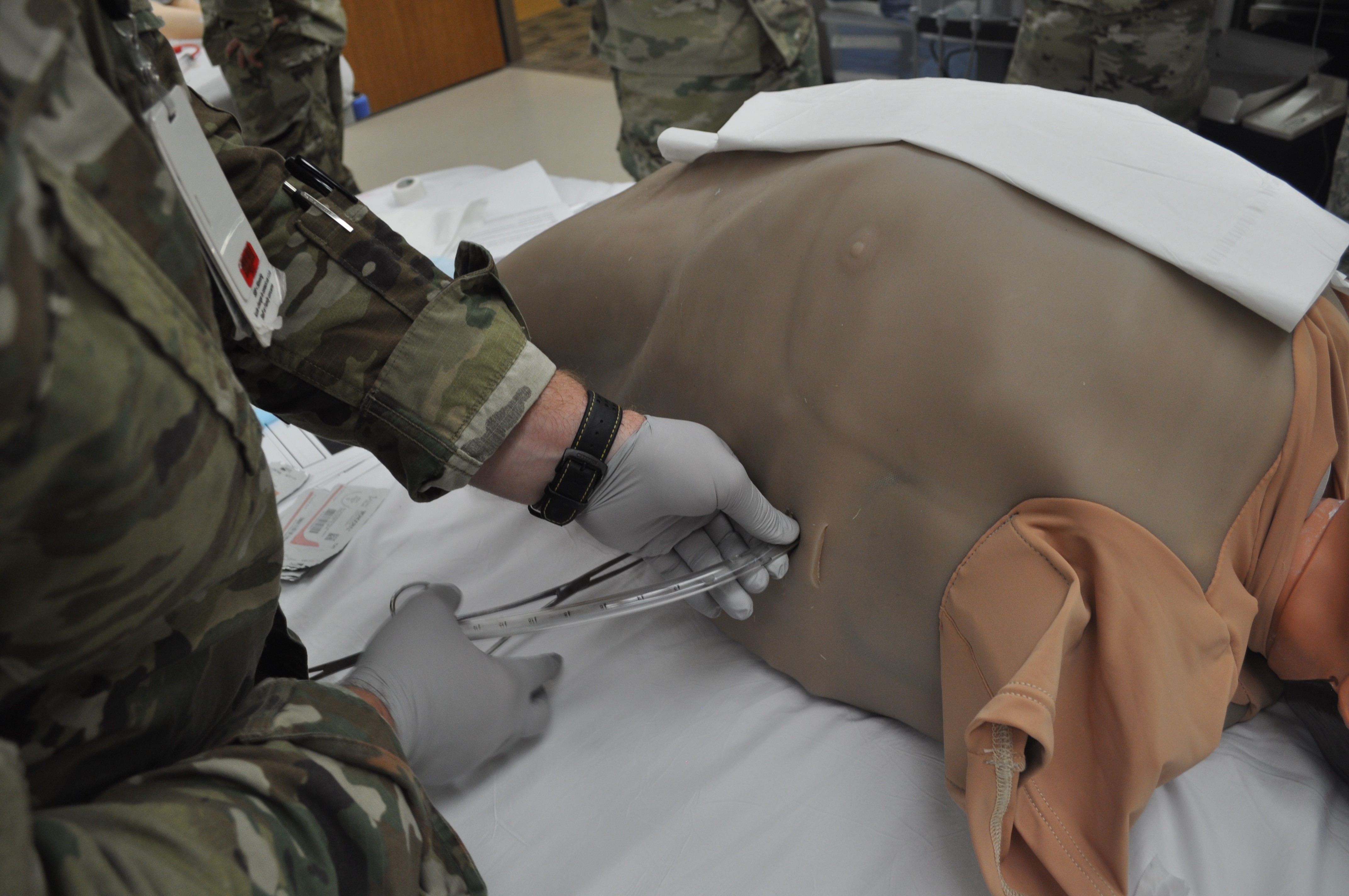
“Take your needle, take it all the way down into the chest wall and aspirate as you go,” continued Arnold. “Once you get to inside the chest wall, you’re going to get either air or blood. And then pull out and dump the lidocaine. This is not a time to skimp.”
Third-year resident Capt. Craig Cromer will be pcs’ing to Fort Jackson to serve as the Brigade Surgeon for the 193rd Infantry Brigade. The new doctor admitted the chest tube simulation was probably the most technically difficult of the workshops.
“We don’t often get many opportunities to practice that type of procedure,” said Cromer. “It was very helpful to have that hands-on training directed by an ER provider who has performed the procedure many times.”
A chest tube is needed when a patient has suffered a severe injury or trauma to the chest wall, to prevent their lung from collapsing. Arnold said in the BMACH ER, the majority of chest tube insertions are done to treat spontaneous pneumothorax [air trapped in chest not due to trauma] in trainees.
“Once you have inserted the tube along the right track … directly over the lower rib taking care to avoid the neurovascular bundle running below each rib … take a deep breath,” recommended Arnold. “You fixed any of the life threatening problems. If they have tension pneumothorax, you just solved it. If they have so much hemothorax [blood in chest] they are dying from that, the blood is just going to start pouring out of the hole.
“The one thing that’s very easy to mess up is if you are nervous or you are amped putting in a chest tube and you just shove it in. You have to put in the chest tube nice and slow.”
In addition to the chest tube simulation, the 3rd-year residents rotated through four other stations, practicing the skills that will be expected of them as deployed field surgeons.
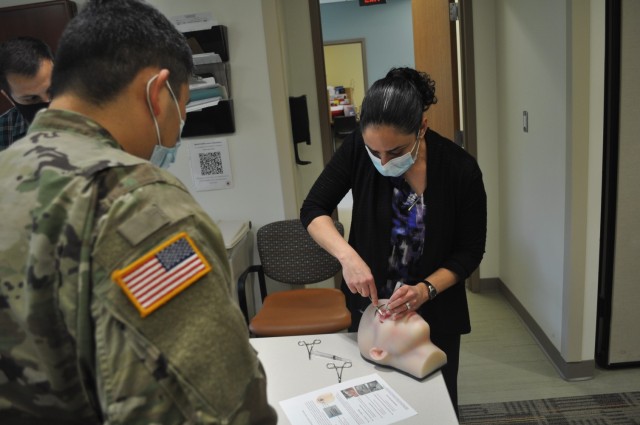
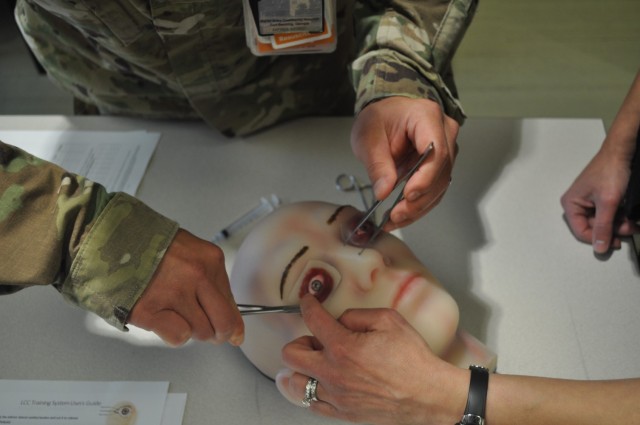
One station gave residents the chance to save a patient’s eyesight after blunt trauma to the face, by performing a Lateral Canthotomy and Cantholysis (LCC). The 5-step procedure quickly releases pressure on the optic nerve caused by sudden bleeding behind the eye.
University of Maryland Medical Center Opthalmologist Dr. Dona Richa walked 3rd-year residents Capt. Cordell Hachinsky and Capt. Mark Betten through the LCC: feel the eye for the telltale bulge, inject anesthetic, crush the tissue to minimize bleeding, use scissors to make a full thickness cut along the upper tendon, then cut the lower tendon to release the eyelid and check for successful decompression.
“If you have local [anesthesia], local is really nice. If you don’t have it, you don’t have it,” said Richa. “What you tell the patient is ‘If I don’t do this procedure, you will go blind. Hold still. I’m going to be putting sharp objects near your eye. Hold still.’’
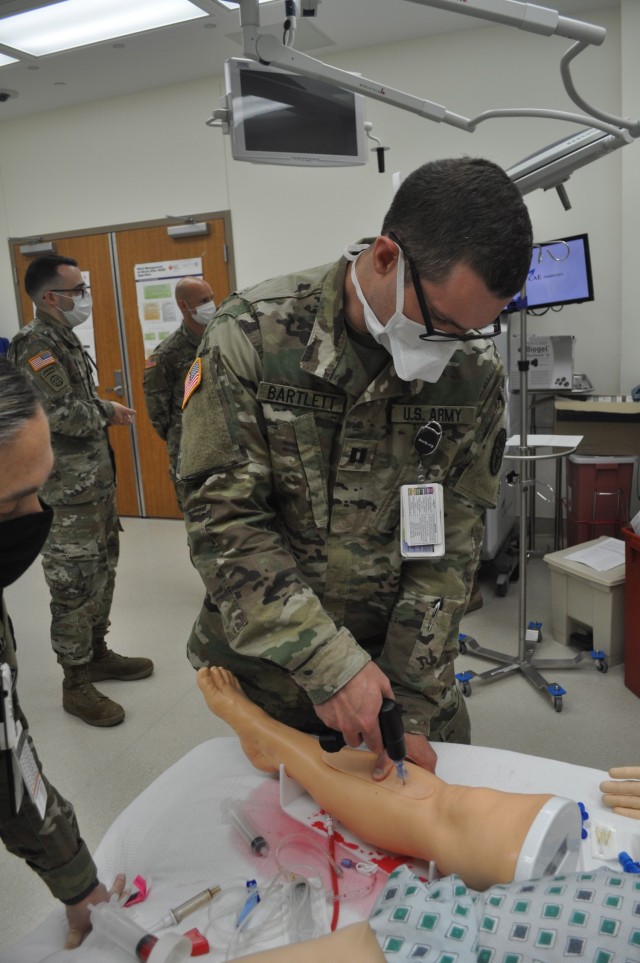
At another station, residents practiced intraosseous cannulation (IO) or drilling a sturdy needle through bone to infuse fluids and blood products to critically ill patients. It sounds horrific, but Sports Medicine Physician Maj. Ben Buchanan said the procedure is fast enough not to necessarily need any numbing agent.
“If you have time and they are not dying you can give them an injection of anesthetic,” said Buchanan. “But if you need to, you just drill. It takes half a second. I would just always do the leg, unless they don’t have legs. Then you look at the proximal humerus (upper arm).”
Buchanan also walked them through a needle decompression (needle D) to quickly but temporarily relieve tension pneumothorax. Chest trauma such as a puncture wound can cause air to fill the cavity, thereby limiting the lung’s ability to expand. Respiratory distress or tanking vitals when there are no obvious signs of bleeding out can indicate tension pneumothorax.
Intern Capt. Michael Dolan served as the patient as residents practiced Extended Focused Assessment with Sonography for Trauma readings. eFAST is an ultrasound typically used in the Emergency Department or in the deployed setting. Third-year residents Maj. Shelley Flores and Capt. S. Ivan Bartlett took turns using the trauma ultrasound to ensure there was no free fluid, in this case blood which shows up as a dark mass, in Dolan’s chest and abdomen.
“It can help us identify potentially life-threatening traumatic injuries such as bleeding, a collapsed lung, or blood trapped around the heart,” said Chief of Emergency Medicine Maj. Benjamin Jennette. “Being able to perform the test [eFAST] during a hectic trauma evaluation while other members of the trauma team are also working in close proximity is usually distracting. This presents a significant challenge for less experienced physicians.”
Strong Team Clinic Registered Nurse Cynthia Avera ran the peripheral IV (intravenous line) starts station. Avera offered tips and recommendations to get a painless stick.
“I want you to learn by feel, the spongy vein is a lot more stable. If you go by sight, a lot of times you will get a vein sitting on top of muscles, they are more likely to roll and move on you,” advised Avera. “When you start an IV, you don’t want the needle at a higher angle because if you do, you are going to stick right through them. The tip of this [needle] is like a scalpel, it’ll go through that vein so quickly and you’ll end up with them having a blown vein.
“You have to be really careful with that. If it does start to blow a little bit, I’ve held pressure on it, just held it there for a few seconds. It’ll close itself off. 99% of the time, it’ll work and it’ll be absolutely fine.”





















Social Sharing