MADIGAN ARMY MEDICAL CENTER, Joint Base Lewis-McChord, Wash. – When a child gets sick, a family is thrown into turmoil. There is confusion, chaos, pain and a substantial amount of fear. In the first month after a startling diagnosis, a family accepts a new reality as the finer details of dealing with an illness reveal themselves. The care team starts a treatment plan and the family begins to get a feel for how things might unfold. Those first 30 days were everything to the Dehn family.
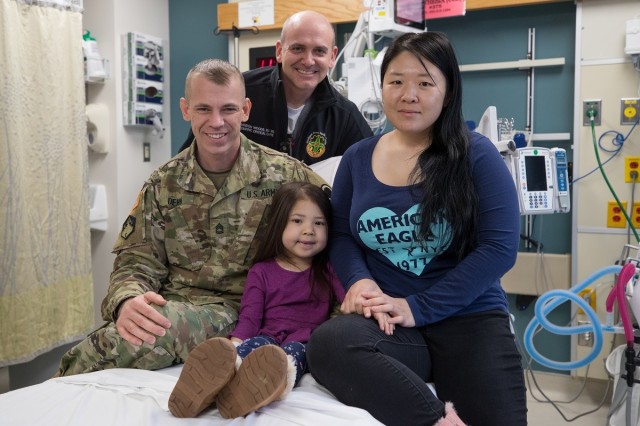
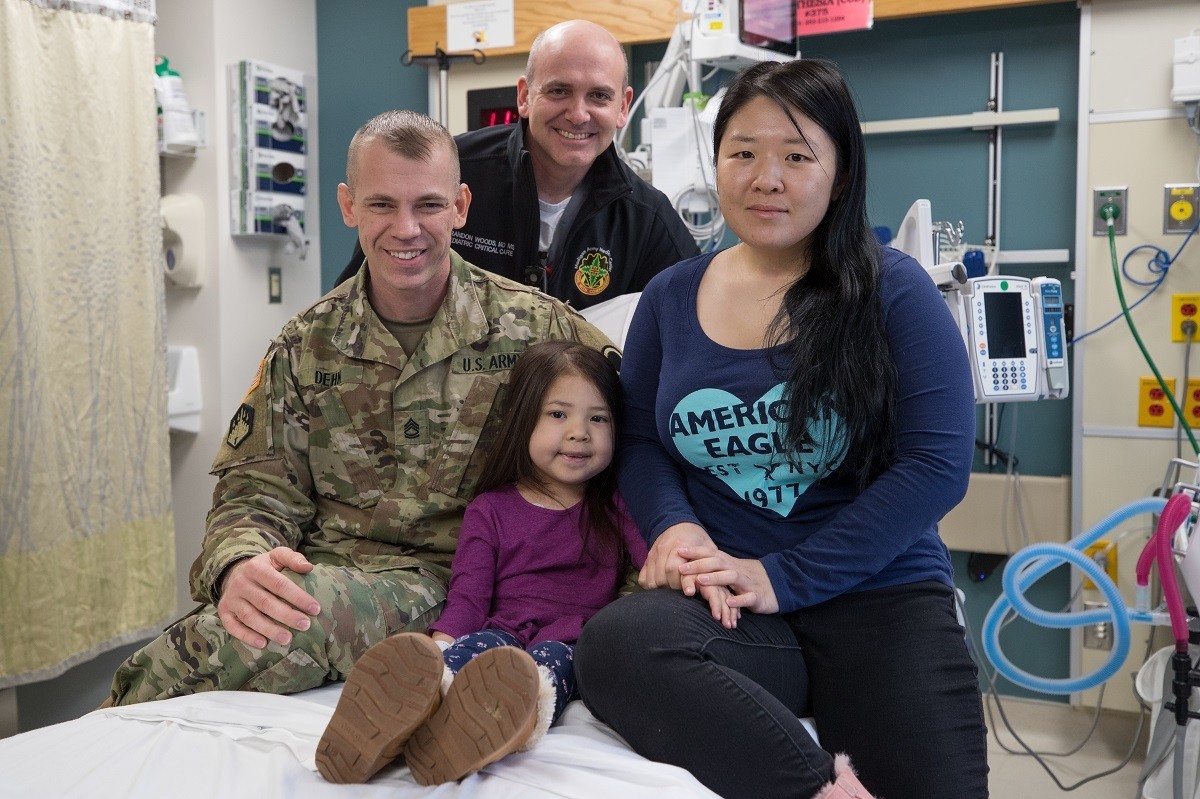
Cora, a shy and petite 5-year-old, isn’t sure why her dad keeps telling people about the rash that developed on her face last October. After getting a call from the daycare on base about it and the fever that accompanied it, her dad, Sgt. 1st Class Christopher Dehn, an inspector general with I Corps, took her to the Emergency Department at Madigan Army Medical Center on Joint Base Lewis-McChord, Wash. She’s spent a lot of time at Madigan since.
After a diagnosis of impetigo, a skin infection, she got some antibiotics and a cream. The rash went away. But, shortly, it returned.
“I was kind of worried about it. So, I brought her back to the (ED); that’s when they did the bloodwork and that’s when we found out that she had leukemia,” said Chris. “That’s when the whole journey began.”
“Her leukemia is B-cell acute lymphoblastic leukemia, B-ALL. It is the most common type of leukemia in childhood; leukemia is the most common type of cancer in childhood,” explained Col. (Dr.) David Harper, the chief of Inpatient Services for the Department of Pediatrics and a physician in the Pediatric Hematology/Oncology Clinic.
Harper also acknowledged that childhood cancers can be a bit elusive at first. Cora’s rash wasn’t entirely unusual as a first presentation of her underlying leukemia, which is a rare condition. It is, therefore, pretty common for there to be a handful of engagements with the healthcare system before a cancer diagnosis is determined.
On that second ED visit, lab work was done to dig deeper into what was causing Cora to feel ill and not be able to heal from the rash.
“After confirming her blood counts, she was quickly admitted to the PICU (Pediatric Intensive Care Unit),” said Maj. (Dr.) Brandon Woods, the medical director of the PICU.
Well under the standard turnaround time, Cora’s treatment was underway.
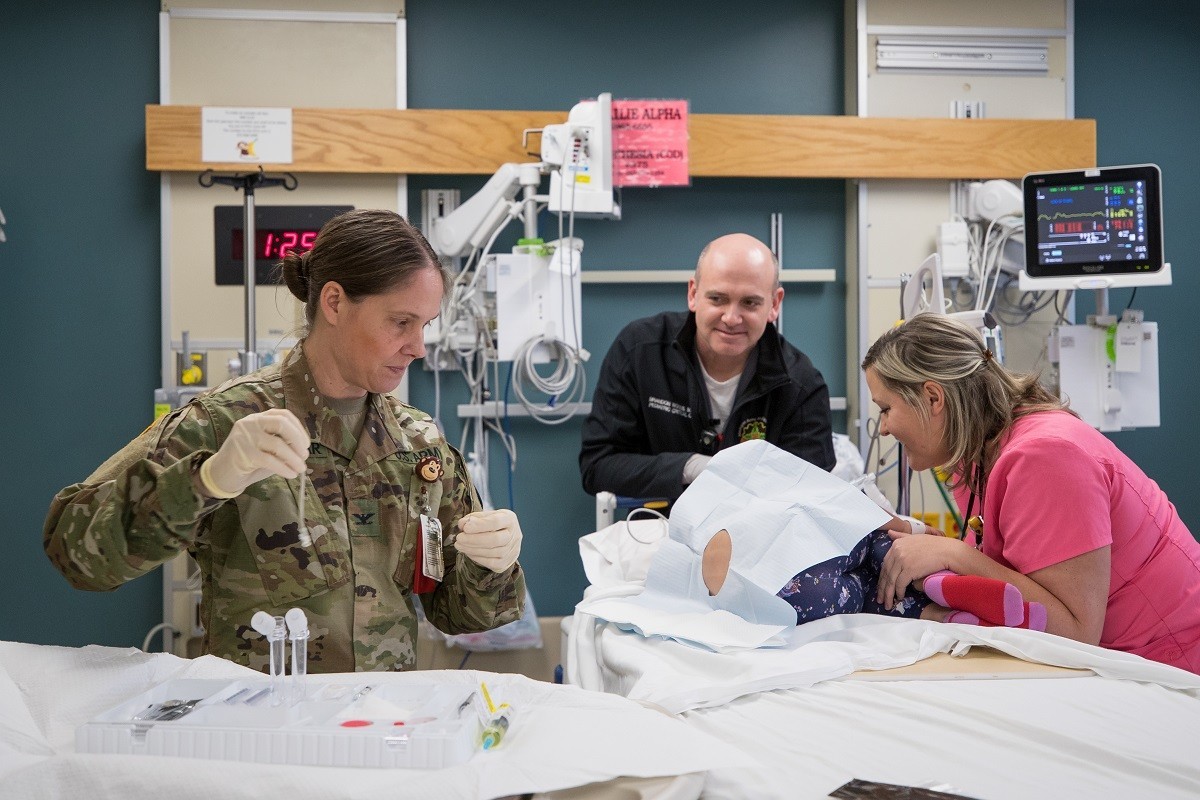
“During her initial 15 hours in the PICU, she received antibiotics, transfusions, a lumbar puncture, a bone marrow biopsy with aspirate to confirm diagnosis, and a PICC line was placed so she could receive chemotherapy,” detailed Woods.
Harper clarified that 15 hours is a short period of time for all of that to occur.
“That requires the institution coming together. We need Lab, Pathology, Pharmacy, PICU and us (Pediatric Hematology/Oncology) all doing things,” Harper said.
Though Cora’s treatment was moving quickly, it was just the time needed for Cora’s mom, Staff Sgt. Eunji Dehn, a cryptologic linguist with 2nd Battalion, 1st Special Forces Group, to make it back home.
“He dealt with this by himself; I was deployed,” said Eunji of Chris who was taking care of Cora and her sister, who is nine, while Eunji was in Afghanistan. “My unit was really supportive, they sent me right away.”
Those early days of Cora’s diagnosis and treatment were a bit of a haze for the family.
“The timeline’s kind of blurry because once we got here, I didn’t sleep for a couple days,” noted Chris. “I also have zero memory; we weren’t in our right minds,” confirmed Eunji.
Cora spent a few days under the watchful eyes of Woods, Maj. Michelle Fredach, a registered emergency nurse, and the PICU team as they helped her clear her infection. Once free of that concern, Cora moved to 4 North for 21 days as her pediatric oncology team got her treatment plan underway.
From ED to PICU to 4N to Peds Hem/Onc, the Dehns found themselves in the good hands of a whole care team committed to their family.
“I came back on a weekend,” said Eunji. “Dr. Harper was like, ‘I will come in, I’m pretty sure you want to hear it from me.’”
“Dr. Woods from PICU as well. I don’t think either one of them were on their shift, but it didn’t matter. When she came back, they both made themselves available to talk,” added Chris.
Cora is doing well now.
“At the end of the one month – the induction phase – they do another bone marrow aspiration to see, and she went into remission at the end of that 28 days. Obviously, she’s still doing treatment to make sure she doesn’t relapse,” said Chris.
As Cora nears the maintenance phase of her treatment, her weekly appointments are set to reduce to monthly.
“We were told to expect probably two to three years for treatment. I know each patient is unique and different,” Eunji said.
The family continues to lean on the whole-family care that helped them through those first days.
“We just do what Dr. Harper and Dr. (Col. Melissa) Forouhar (the chief of the Pediatric Hematology/Oncology Clinic) say,” admitted Eunji. “She’s doing great. No severe reaction as far as any of the chemo meds she’s exposed to so far, so we’re grateful for that.”
Not only did Cora’s treatment get underway quickly, it has proven a bellwether too.
“Over 90 percent of kids with the kind of leukemia she has will be cured,” Harper explained. “But, an important part of that is treating the central nervous system so the leukemia doesn’t come back there. We do that with chemotherapy, but we have to give it into the spinal fluid. So, they get a lot of spinal taps.”
The standard of care for that procedure has been to sedate children using the drug propofol.
“We don’t know the risks of multiple propofol sedations long-term. Kids who have been treated for leukemia overall have an increase in incidence of attention problems and some other problems later on and we don’t know if that’s medications or if that’s sedations, or all of these things together,” described Harper.
An alternative to propofol is nitrous oxide. Many people know it from getting it in the dentist’s chair as a kid themselves.
Madigan’s Sedation Service has developed the use of nitrous oxide in a number of areas in the hospital to include in obstetrics for laboring moms. The service has been growing its use with kids as well. Cora was the first patient to try it out during a lumbar puncture.
Having first used it on her to biopsy her rash, her care team went into a lumbar puncture with a plan to use it and have the propofol ready should the nitrous oxide not work well.
“But, it went very well,” said Harper. “We’ve now offered this to other families.”
Madigan is, in fact the only military treatment facility that offers nitrous oxide for pediatric patients, added Woods.
“By utilizing nitrous oxide, she does not have to be fasting prior to her procedures,” Woods said.
Harper noted that, unlike with propofol, she remains conscious and is able to respond. Plus, her recovery from each procedure is quicker, making the next few years she will be having these treatments less daunting.
From those anxious first days to leading the way for cancer care for other kids, Cora’s situation is looking up.
“That first month when we didn’t know what was going on. Now, we’re more hopeful because she’s doing so great,” said Eunji.
Madigan’s Social Media Links:
Madigan’s Facebook:
www.Facebook.com/Madiganhealth
Madigan’s Twitter:
www.Twitter.com/Madiganhealth
Madigan’s Instagram:
www.Instagram.com/Madiganmedicine
Madigan’s LinkedIn:
www.Linkedin.com/company/madigan-army-medical-center/
Madigan’s YouTube:



Social Sharing