FT. WAINWRIGHT, Alaska - In preparation for patients who may need intensive care due to COVID-19, Bassett Army Community Hospital has converted patient rooms to meet intensive care unit standards.
We are planning for a worst-case scenario,” said Lt. Col. Victoria Ragan assistant deputy commander for nursing. “We are ready to support in the event all the ICU beds in Fairbanks are full and we are needed.”
The rooms, located in the multi-service unit, required changes to venting, airflow, equipment, and additional staffing; a project that needed the assistance of multiple departments within BACH.
Staff from facilities installed high efficiency particulate air, or HEPA filters, and converted the rooms to negative pressure. Negative pressure allows air to filter into the room but not escape, preventing airborne contagious diseases such as COVID-19 from contaminating other parts of the unit.
With the rooms converted to negative pressure, shifting of equipment within the hospital was necessary.
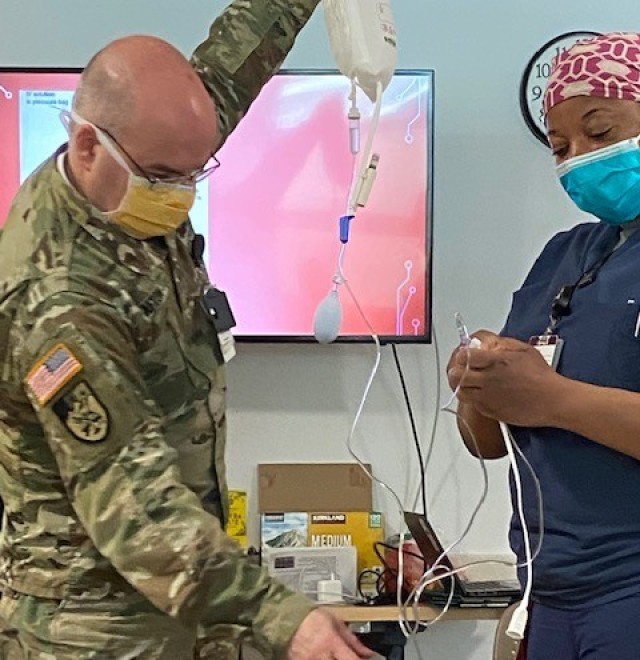
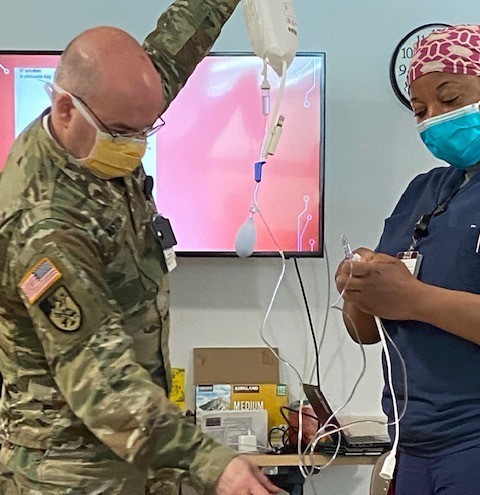
“We had the majority of the equipment on hand for emergency situations, but only in small quantities,” said Ragan. “We had to shift a lot of things around within the hospital to support the ICU beds. Some of this equipment includes ventilators, heart monitors, additional IV pumps, and extra oxygen and suction capabilities, said Ragan.
The completion of physical changes to the ICU rooms took a week to accomplish, while training of staff to work with COVID-19 patients and in an ICU is ongoing.
Ragan, an ICU nurse herself, worked with departments to identify nurses and providers with previous ICU experience. These staff members are continuing training to solidify procedures and implement COVID-19 specific protocols.
To assist with training and ICU patient care, BACH received ICU nurses from military hospitals outside of Alaska as well as to Air Force nurses from Eielson Air Force Base here in interior Alaska.
“I’ve been really humbled by the amount of staff that stood up and volunteered to train for and care for COVID-19 patients,” said Ragan. “As a group we talked about the risk to our own health with exposure to high viral loads. In the end it always came down to, ‘I’m a nurse or doctor and when people need me I have to be there and try my best to help’ from those volunteering.”


Social Sharing