When she gets on a roll at the podium, Behavioral Health Epidemiologist Katie Nugent strikes a tone so laced with raw, vibrant energy that it's almost impossible for the audience to sit still. It's the kind of passion that can only come from a true believer -- a person who feels the weight of their work with every single statement they make.
"When we talk about behavioral health we're talking about first responder care," said Nugent, succinctly addressing a substantial crowd during her lengthy presentation at the 2019 Military Health System Research Symposium in Kissimmee, Florida. "And our research shows that we need to adapt our delivery techniques for far forward areas."
Indeed, for years researchers like Nugent have struggled with the so-called 'empty toolkit' problem: the fact that behavioral health providers have fewer options for care --fewer tools at their disposal-- for Soldiers in far-forward areas. In simpler terms, that means said providers have precious little in terms of capability to either identify or care for emotional responses like loneliness, depression, or other altered mental states the closer they get to the combat zone. Add to that mix the military's current preparations for future battlefield scenarios that will likely expand the very concept of the combat zone altogether, and the potential for greater behavioral health problems amongst America's Warfighters becomes very real, according to researchers.
"Any limitation to one particular soldier is going to impact what the overall unit can do," said LTC Justin Curley, one of Nugent's research partners who is also based out of WRAIR.
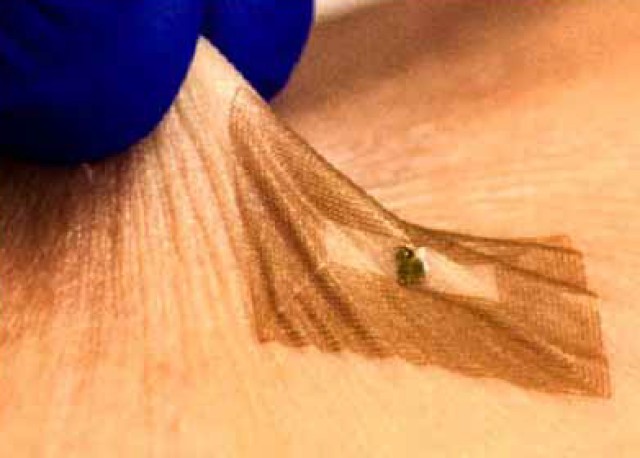
To that end, one of the dominant themes of Nugent's research --as well as, in fact, the larger world of far-forward behavioral health innovations-- is the development of solutions based on the study of the actual human combat experience. The three-point plan she outlined to her audience at MHSRS will eventually rely on data gleaned from both individual interviews and large-setting focus groups; with both efforts targeting Soldiers who have previously been deployed in a variety of settings to answer questions about the depth of their current and previous behavioral health training. In a slight departure, the third leg of Nugent's effort will be technological in scope; specifically, she hopes to make use of wearable sensors and smart phone applications --in short, non-pharmacologic solutions-- to load that theoretical 'toolkit' with materiel and knowledge products that can help any medic at the point-of-injury make the proper decisions for the sake of future psychological readiness.
Said Joshua Wilk, another of Nugent's colleagues at WRAIR, "We're really casting a wide net with regards to pairing here so we don't miss anything - and also so that we don't repeat any efforts."
Meanwhile Nugent is, predictably, moving full-steam ahead with her endeavors. She's already collecting data on the aforementioned interview efforts, and hopes to test and validate that data in the next three years. For her it is imperative --a personal requirement, even-- to translate all that energy into a new and better tomorrow.
"The goal is to return Soldiers to duty as quickly as possible," said Nugent in closing, "and so we need to ask ourselves what we can give them to help them recover."

Social Sharing