CAMP BULLIS, Texas -- The U.S. Army continuously looks to new technologies and test new devices to increase battlefield survival rates. Recently the U.S. Army Medical Department Board conducted a test on an intrathoracic pressure regulation therapy (IPRT) device that researches hope will help save lives of the critically injured.
The IPRT device increases blood pressure and circulation to tissues of the body in ventilated patients who have low blood volumes. Cleared by the Food and Drug Administration, the IPRT noninvasively decreases intrathoracic pressure leading to an increase in blood circulation. It is beneficial for patients who have compromised blood flow from shock, high pressure in the brain, and other low-perfusion conditions. The IPRT apparatus is connected to the breathing circuit of a ventilated patient, and it is beneficial for patients who have compromised blood flow from shock, high pressure in the brain, and other low-perfusion conditions.
Sgt. 1st Class Jacob Horspool assigned to the AMEDD Center and School, Health Readiness Center of Excellence in the AMEDD Board, served as the noncommissioned officer in charge of the test. "The device draws blood back into the heart and lungs while at the same time decreasing pressure in the brain that caused swelling," said Horspool. "If a patient has a good pair of lungs we can use this device to bring blood back without having to add additional fluids that can water down the blood," He continued.
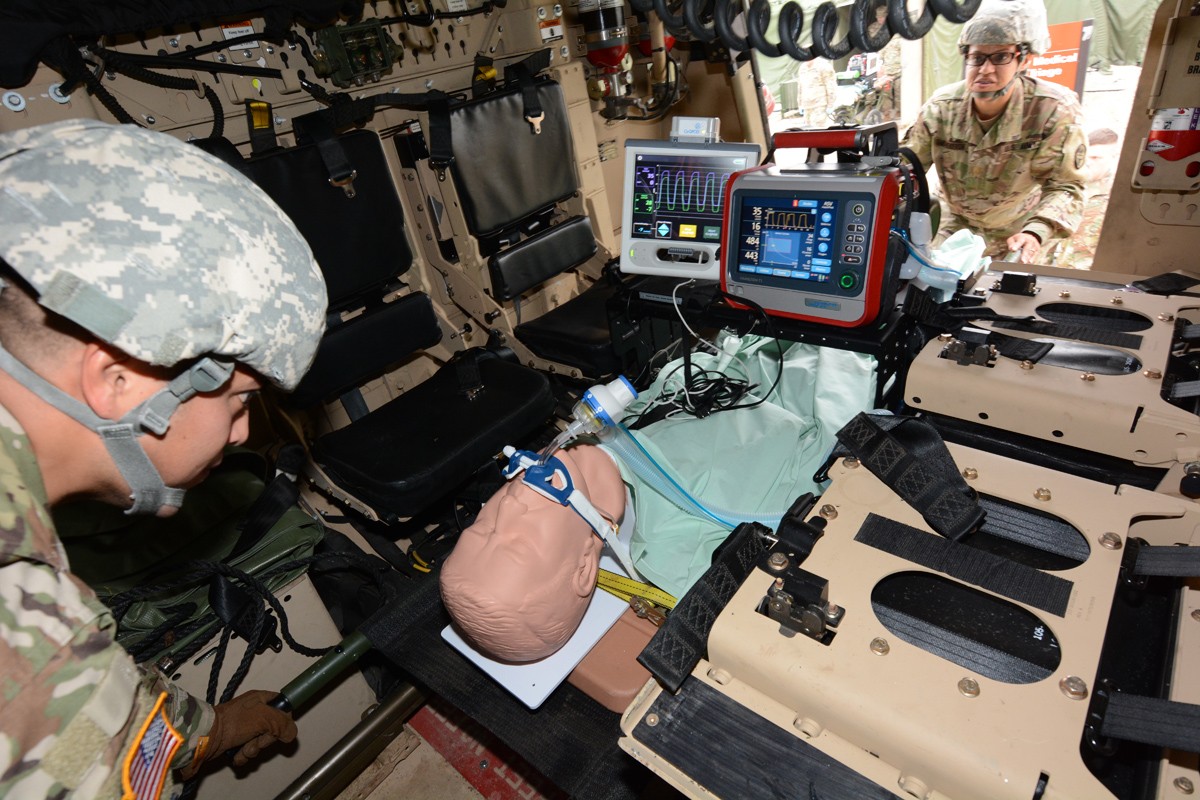
Soldiers from various Army medical units served as test players during the operational test in a simulated real world deployment scenario. For the test, the AMEDD board brought in potential IPRT users; a pulmonary disease officer, emergency medicine physician, physician assistant, nurses, combat medics, operating room specialists, paramedic/aero MEDEVAC specialists, and respiratory specialists. Conducting the test at Camp Bullis allowed the team to use the device on various power sources within a combat support hospital and aboard field ambulances.
Chief Warrant Officer two Goldie Cooper assisted with the tests and is also assigned to the AMEDD Board. Cooper said that getting the mechanism field tested is an important first step to getting them purchased and added to the Army inventory. He stressed that operational testing is where the Army identifies whether the device is suitable for use in an operational environment.
It is estimated that 90 percent of potentially survivable deaths (approximately 1,080) in Operation Iraqi Freedom/Operation Enduring Freedom were caused by hemorrhage and hemorrhagic shock. Spanning all documented wars, hemorrhage and hemorrhagic shock have been the leading causes of service personnel killed in action. Cooper said, "Ultimately it's about survival rates, and restoring lives on the battlefield. Every minute is valuable when we're trying to save lives."
Once the testing is complete, the AMEDD Board test team prepares a summary report that assesses the IPRT's suitability and effectiveness. The device will go through several reviews to ensure it will meet the Army's needs prior to approval and deployment.
To learn more about the AMEDD Board or other HRCoE initiaves visit http://www.cs.amedd.army.mil/.







Social Sharing