JOINT BASE LEWIS-MCCHORD, Wash. (Oct. 11, 2018) -- Medics are trained for the immediate care of the injured, wounded and seriously ill. Caring for patients for extended time periods or performing complex procedures have not traditionally been a significant part of their training. As medical techniques and equipment are pushing the bounds of their lifesaving capacity and aid is rendered in more and more austere locales, medics are required to do more before handing a patient off to the next level of care.
The need to nurse in addition to aid and transport is opening more capabilities for advancing technology to step in and assist. Tele-health capabilities are putting expert eyes on patients from afar and connecting the on-scene responder with subject matter experts for support and mentoring.
Two exercises within a month's time afforded Madigan Army Medical Center's Virtual Critical Care Center opportunities to get in the game remotely and test potential uses for equipment.
Lt. Col. (Dr.) Christopher Colombo, the director of Virtual Health and Telecritical Care and an intensive care physician, was at the center of both of these activities.
To him, remote medicine is a boon to providers and patient care.
"It aids and provides more staff to the task-saturated situation with overwatch capabilities of virtual critical care," he said.
Within the hospital itself, cameras in the patient rooms and a medical professional to monitor them, "adds a layer of quality and safety," said Colombo.
Inserting telehealth capabilities into field exercises offers the proof of concept and further testing of equipment that are expanding the use of telehealth options.
The Army Best Medic Competition was held at Joint Base San Antonio in Texas Sept. 16 through 20. The competition incorporated a telemedicine option into its prolonged field care scenarios. The competitors were given cards with information on ADVISOR -- the Advanced Virtual Support for Operational Forces synchronous teleconsultation line. They could choose whether to reach out or not during their scenarios. They made heavy use of the option to phone an expert.
In tandem with providers at Brooke Army Medical Center, in San Antonio, and the Telemedicine & Advanced Technology Research Center, at Fort Detrick, Md., Colombo and another Madigan staff physician fielded calls from 27 competitor teams during "open comms" periods in their exercises. Madigan's doctors provided six hours of call coverage and fielded 25 calls, giving advice, information and mentoring on topics ranging from polytrauma, burns, disease and non-battle injuries, diagnosis and management of low blood pressure, pain management, nursing care, and general medical knowledge.
The main piece of this connection was a simple phone conversation. There was, however, always the ability to send and receive photos, videos and documentation as all participants were using smartphones.
This allowed Colombo to put his feet up, enjoy his evening and still share his expertise.
"This is fun for me," he said. "It's work on their end. They're in a mud hut with a red light."
Moving well along the technological path was the next exercise on Madigan's VCCC schedule -- a joint exercise with the Navy for Fleet Week.
Devised by a small group of telehealth specialists across facilities and services, the Oct. 3 exercise presented a scenario of a team of first responders and casualties simulating a seismic event occurring on Treasure Island in San Francisco Bay. The first responders were firefighters and emergency medical technicians with expert trauma care skills but no, or very limited, surgical skills.
The scenario assumed that time and distance -- two factors that complicate battlefield medicine -- rendered it necessary to perform prolonged field care and onsite procedures beyond the usual scope of emergency response medicine.
Madigan's part of the exercise engaged the VCCC to remotely monitor the vital signs of 20 patients onsite in the Bay Area. Patients were given finger-mounted devices that monitor blood pressure (with the use of a cuff), pulse oxygenation, and heart rate. These transmit the information to a tablet on scene as well as the web-based application that Colombo and Kristina Ieronimakis, a registered nurse in the intensive care unit, observed in the VCCC.
A bit past the appointed hour, Colombo's cellphone emitted a sea horn, alerting those gathered that the Navy was ready to play.
"Roger that. I can take over overwatch," relayed Colombo on the call.
Once Colombo received the call, he dialed up a videoteleconference link with Naval Medical Center San Diego that is permanently connected via the Joint TeleCritical Care Network between Madigan, NMCSD and the virtual medical center at BAMC.
Ieronimakis refers to this link as her "window to the world" that she says keeps her from feeling alone.
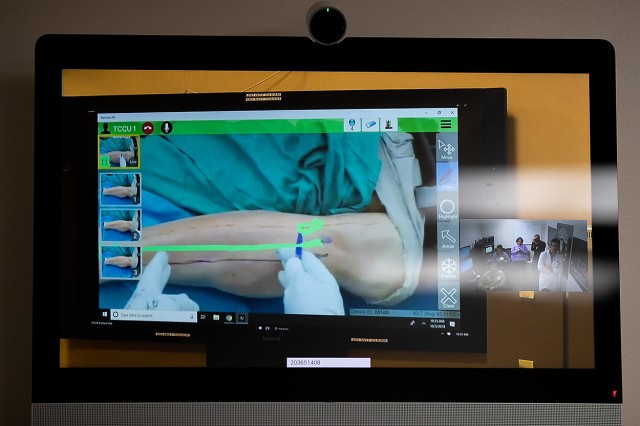
Colombo, Ieronimakis and observers watched the team assembled at NMCSD as an orthopedic surgeon walked a first responder on the scene through a fasciotomy -- a surgical procedure on a casualty's leg to relieve pressure and keep the leg from dying from restricted blood flow.
Viewing the multi-site exercise drew expressions of awe as experienced physicians in the Madigan VCCC watched a firefighter perform a procedure the parts and equipment of which, such as making the necessary incision and using a spreader to hold the skin open, he had no experience with at all.
The first responder wore augmented reality headgear that was connected to the surgeon's transportable exam station. The surgeon saw exactly what the firefighter saw. As the responder looked at the set of tools he had on hand, the surgeon told him which to use, such as third scalpel from the left.
The surgeon drew on his own screen to give the responder reference points. The responder saw those through his lens as he looked at the patient. He then transferred those marks onto the patient's leg. With the scalpel, he followed the incision line he just drew, following the surgeon's marks, as the surgeon and other team members watched.
One of the questions of telehealth's place in the hospital is how does it fit in with traditional care.
"It's the mindset of instead of this taking away or replacing the bedside provider, it's the adjunct that allows the bedside provider to get back to what they're supposed to be doing, which is caring directly for the patient," said Colombo.
Through exercises and everyday care, telehealth puts Madigan's physicians and nurses anywhere they are needed -- from the bedside to the rubble pile.













Social Sharing