People tend to think youth brings the peak of physical health. As the human body ages, that's when conditions set in that deteriorate health.
Keratoconus flies in the face of this thinking. It is most commonly found in teenagers and young adults.
"My vision with my left eye was rapidly declining. Every time I went to the eye doctor, it was a new prescription for my left eye," said Sean dela Pena on his experience with keratoconus. Sean is a high school senior whose mother, Maj. Ernestina dela Pena, is a nurse in the Primary Care Service Line at Madigan Army Medical Center.
The condition is a progressive thinning of the collagen fibers of the cornea -- the flat surface of the eye. This produces a lack of strength that leads to an abnormal shape.
Lt. Col. (Dr.) Patrick Munson, the chief of refractive surgery at Madigan, explains that the cornea "Starts to warp and bow; it doesn't hold its normal shape." Instead of a rounded dome, the surface of the eye becomes more of a rounded cone.
The result can be blurry or double vision, nearsightedness, astigmatism, increased light sensitivity and, in the worst cases, blindness.
For Sean, the diagnosis was a bit scary. "The doctor told me that if it does get worse, a transplant is required," he said.
At 5-10 a year, corneal transplants are among Madigan's more common types of transplants. Since keratoconus is a bar to enlistment, the rate of occurrence is much lower within than outside the military. Most of the patients seen by military treatment facilities for the condition are, like Sean, dependents of active duty; some are retirees.
According to the National Eye Institute, which is a part of the National Institutes of Health, keratoconus is the most common corneal dystrophy -- degeneration of tissue of the cornea -- in the U.S., affecting one in every 2,000 Americans.
In the past, there was no treatment for the disease. The symptoms were managed until corneal transplant was necessary to retain or restore vision.
"Now, with corneal cross-linking we have our first therapy to treat that disease rather than just the symptoms," said Munson.
"The crossing itself involves creating more and more cross-links between the collagen fibers in the cornea to strengthen it," Munson said. "If you've got support struts, you're now putting cross beams to connect them."
In the months after the diagnosis, Sean and his mom looked at their options. When they found cross-linking, they knew that they had to do it.
Initially looking into treatment in Seattle before the procedure was offered here, dela Pena found that she would need to take Sean to the clinic there for numerous follow-up visits after the procedure itself. Dela Pena noted, "Having the machine here is really convenient for us."
This new procedure was approved by the U.S. Food and Drug Administration in April 2016 after clinical trials. Fort Belvoir, the main eye research center in the Army, was the first Army site to start using this treatment. Madigan is the second.
The cross-linking procedure mimics what naturally occurs with aging by saturating the eye with riboflavin (vitamin B2) and exposing it to ultra-violet radiation -- UVA light, also known as sunlight. This intensive dose of the vitamins and UVA exposure spurs the formation of those cross-linked fibers that strengthen the cornea.
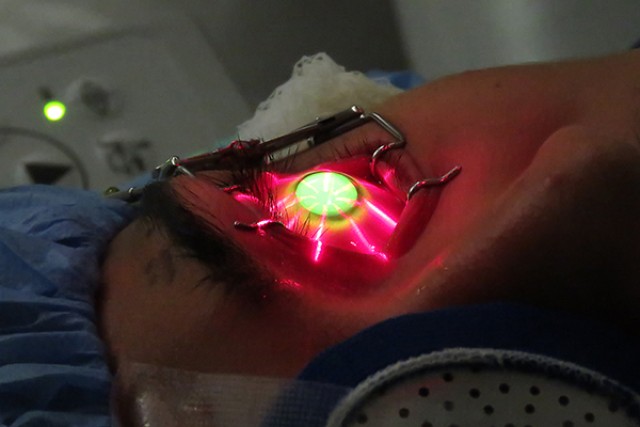
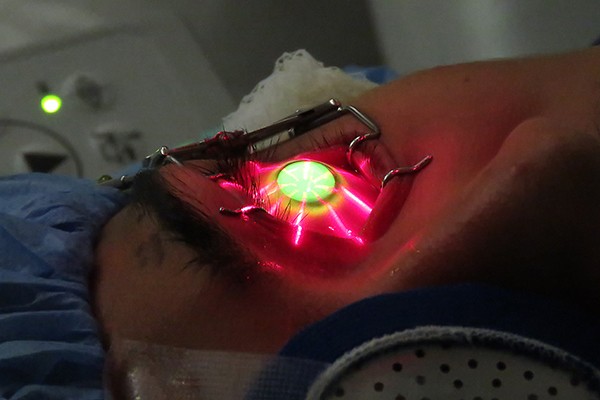
Sean was given a mild sedative before the procedure and some numbing drops. Col. (Dr.) Mark Torres, Madigan's cornea specialist, removed the epithelium -- the "skin" of the eye -- and measured the cornea to determine if it was presenting the right conditions to proceed with the treatment.
From there, Sol Epistola, an ophthalmic technician, kept constant watch over Sean to administer the vitamin drops every 2 minutes for a 30-minute course. "He made sure I was OK," affirmed Sean, adding that Epistola asked how Sean was feeling and if he needed more numbing drops throughout.
Following the course of drops, Sean spent another 30 minutes with his eye exposed to the UVA light. The final step of the process involved Torres putting a contact "bandage" on the eye.
Sean found the contact uncomfortable during recovery. "The whole time it felt like something was in your eye and you just wanted to take it out." Still, just weeks after the procedure, Sean is noticing improved vision in his left eye.
Munson said these procedures have a success rate of 80 percent or higher. Some studies show rates above 90 percent. Though it is expected to be a one-time treatment, if it is not initially successful, it can be repeated.
Success is defined as stabilization. "Our goal is to grab the patient who can still wear the glasses or contacts and treat them then to stop the progression," Munson explained. This is one reason to get in early for evaluation. Munson stressed the options for dealing with all sorts of eye conditions are more extensive at Madigan than many people might realize.
Asking about his prognosis, dela Pena learned that, unlike before this treatment, Sean will be able to wear contacts and even get LASIK surgery after he has his right eye treated and both eyes heal fully.
All of this is very good news to Sean. He is going to college in the fall to study aerospace engineering. "I'd love to build rockets and do what I can to contribute to the greater picture."
That is a goal that can take proper shape now.
Social Sharing