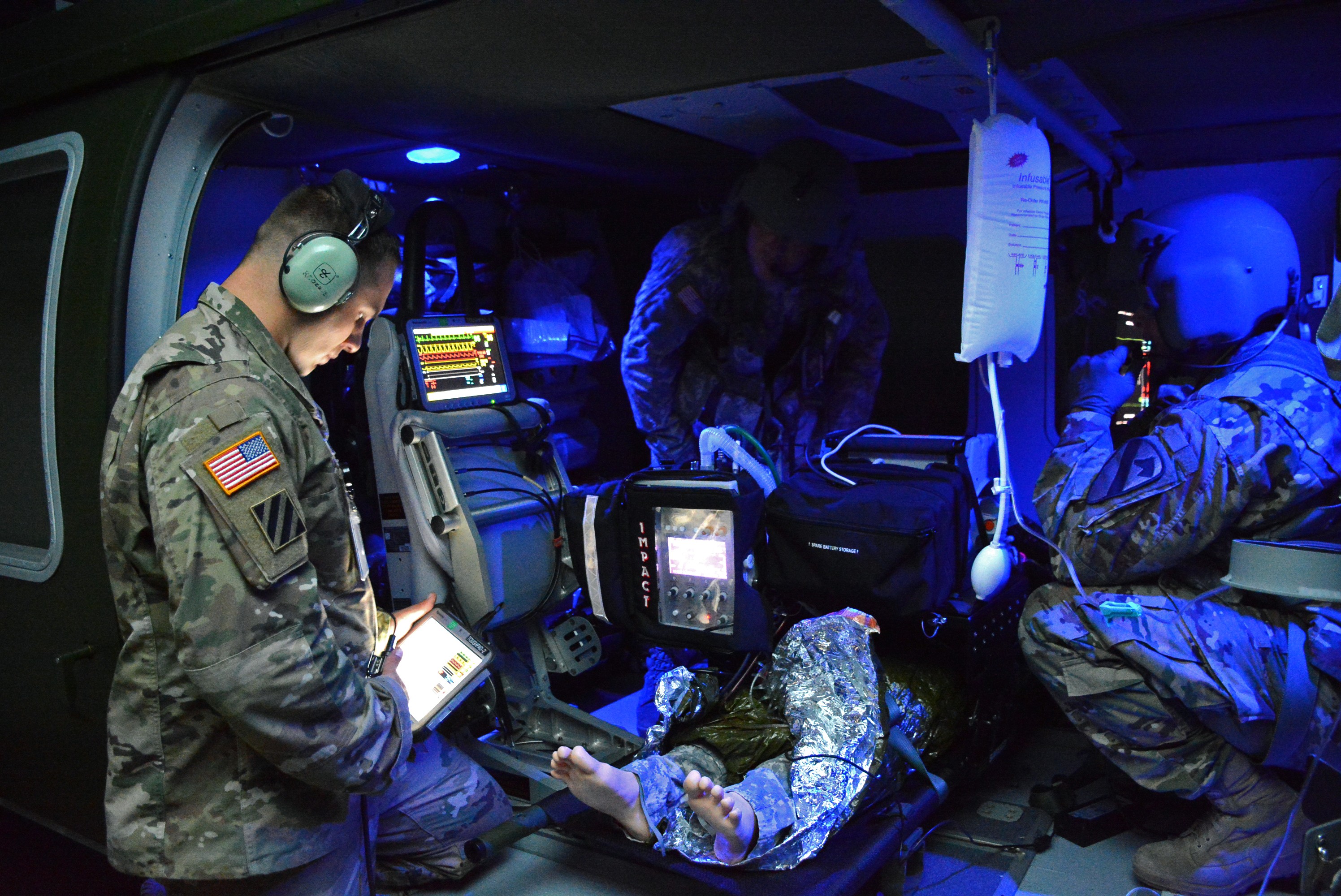
The Flight Paramedic Recertification Course is intense, stressful, fast paced, and most importantly realistic. So realistic in fact that Sergeant Marty Anderson, a certified emergency medical technician (EMT) and member of the Michigan National Guard attending the course said, "Being inside a helicopter trainer is very different than being in the back of an ambulance. We're wearing full battle rattle, it's dark, loud, and windy. The intense exercise feels likes a real helicopter with a live patient," said Anderson describing the experience of treating an injured patient inside a UH-60 Blackhawk trainer. Sergeant Anderson is no stranger to emergency medical care. He works as an EMT in Lansing, Michigan. Emergency care is what he does for a living when not serving with his unit Detachment 1, C Company, 3-238th Aviation Battalion. Anderson recommends that every flight paramedic in the U.S. Army attend the course. "I am so glad I came to this class. I'm taking what I learned to my civilian job and Guard unit."
Taught at the U.S. Army Medical Department Center and School (AMEDDC&S) the course provides Army enlisted Health Care Specialists (68W), who are paramedic qualified, two-weeks of training required for paramedic recertification to include 72 hours of continuing education units accredited by Army Emergency Medical Service (EMS). Additionally, students who are flight paramedic certified through the Board of Critical Care Transport Paramedic Certification (BCCTPC) qualify for continuing education units.
Practical exercises include airway management, treatment of extremity trauma, treatment of combat chest wounds, and lifesaving emergency surgical skills on high fidelity simulation manikins. Students conduct scenarios in both clinical environment and high fidelity aircraft environment. All training scenarios and exercises refresh critical care knowledge and provide recertification.
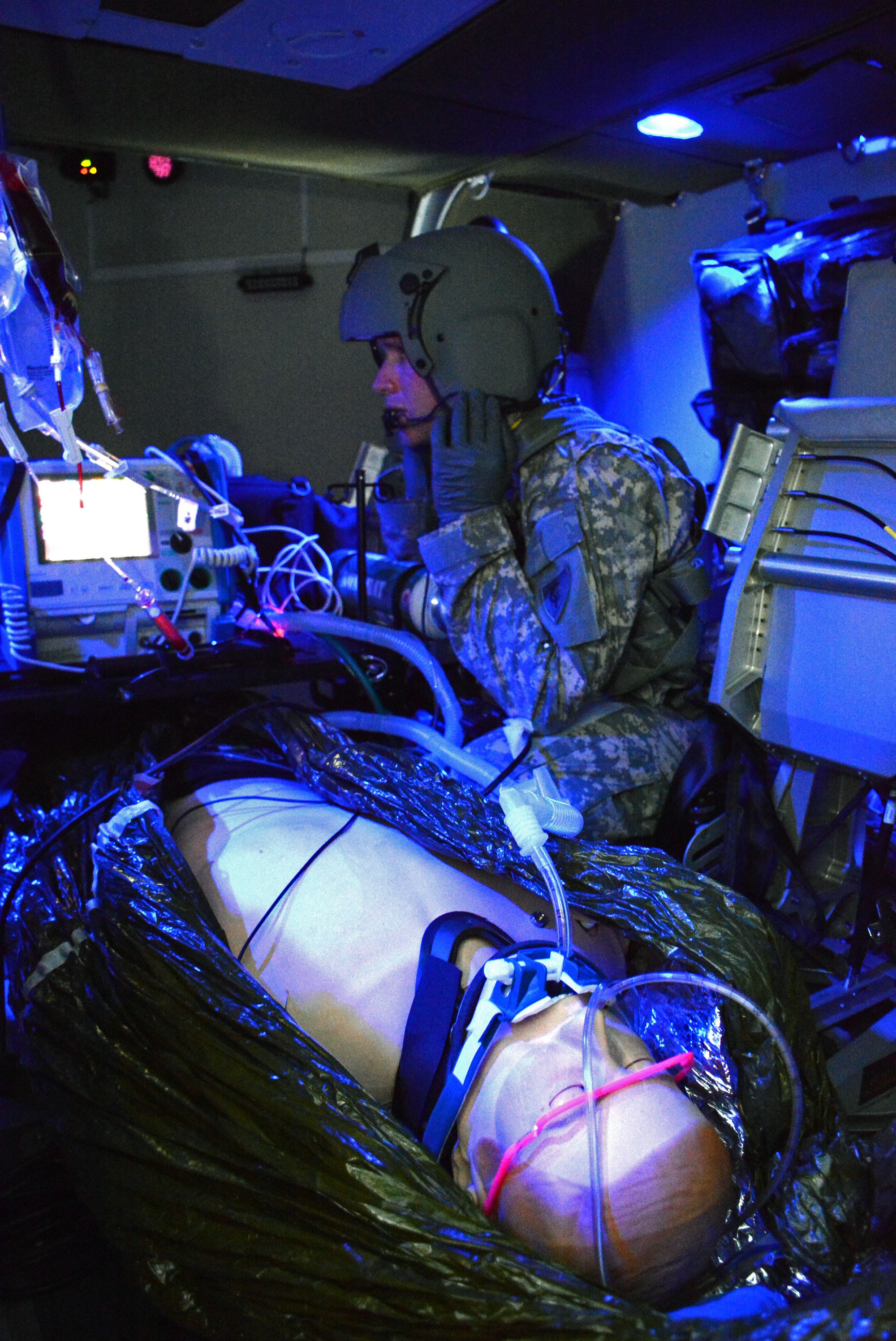
AMEDDC&S is using the most advanced hands-on medical simulators ever made. Synthetic human simulators constructed from polymer composites are replacing tissue in medical education with a realness not possible with older rubber manikins. These innovative devices mimic the mechanical, dielectric and physicochemical properties of relevant living tissue. The skin, organs, ligaments, cardiovascular system, nerves, bones, and flesh textures look and feel authentic, based on actual live tissue tests to mimic the properties of living tissue with an unmatched level of fidelity. These simulators even have beating hearts, breathing lungs, moving limbs, and even pump simulated blood through arteries and veins.
Students can insert their hands and medical instruments then pull back internal body parts for detailed examinations. Tissues respond to all known imaging techniques and medical devices just like live tissue. The materials are about eighty-five percent water, and to prevent dehydration the training simulators are stored in tanks with recirculating fluid. Wireless integrated computer interfaces include controls proving students with vital physiological information on untethered tablets.
These advanced systems are better suited for a new generation of Soldiers who have grown up with Smartphones. The medical patient simulators used at AMEDDC&S have come a long way from the old CPR Annie manikins from the past. While those training manikins were hard plastic, featureless device, more like a department store manikin, today's systems are so life-like, even seasoned instructors have difficulty distinguishing them from real tissue.
The Training Mobile Transport Lab, a life-sized UH-60 platform, offers students stressful experience of being inside a real helicopter with sound, wind, and smoke. Instructors conduct nighttime training scenarios, where flight paramedic students treat patients inside the cargo compartment. The training prepares flight paramedics to load and unload patients on litters and treat them in flight. The training exercise is fast paced and realistic, testing students ability to treat injuries while transporting patients.
Along with the practical classroom exercises, students take part in interactive lectures from insightful subject matter experts, or SMEs, on a host of medical topics. "The small block lectures are phenomenal. We're learning from SMEs with real life experience. This training supersedes anything they received in initial 68W training," said Sergeant Anderson.
As traditional classroom, online, and practical training methods advance, AMEDDC&S continues to invest in new methods and technologies, while preserving the tried and tested techniques that have led the U.S. military having the highest combat survivability rate in history.
Until recently 68Ws could only provide immediate first aid while preparing the wounded for transport to a military field hospital facility. A gap existed between treatment at the point of injury and transport to a treatment facility. In the civilian world, air ambulances provide on-scene and in-transit treatment with dedicated, specially trained, and certified flight paramedics. Yet the U.S. Army lacked this life saving ability. To close that gap, AMEDDC&S established the Critical Care Flight Paramedic Program. Now Army helicopters are more than flying ambulances shuttling the injured to a military treatment facility. Advanced trauma management is accessible at or near the point of injury and while flying to a treatment facility.
"I think about how it must have felt to be a flight medic without skills to help an injured Soldier beyond basic first aid," reflected Major Ersan Capan, the officer-in-charge of the Critical Care Flight Paramedic Program, Transport Medical Training Laboratory. "How horrible it was for an Army medic to see critically injured patients and not have the skills to treat them. To take that with them for the rest of their lives. In the past these 68Ws were little more than part of a flight crew with basic medical training. Now we are giving our 68Ws the skills to provide in flight critical care, similar to civilian helicopter flight paramedics," said Capan. He and his team were instrumental in standing up the curriculum for the flight paramedic recertification course.
"We want our students knowing they did everything possible to save lives, and not to think about what they couldn't do," said flight paramedic instructor Sergeant First Class Reid Carpenter. "We give 68Ws capabilities to meet Army needs. To maintain their skills flight paramedics need to continuously train when back at their units. These Soldiers are more than just part of a flight crew; they are now front line critical care medics. There is an overlapping of skills, almost like a hybrid of combat medics, physician assistants, and nurses. These 68Ws also understand medications. Once they complete the course Soldiers then serve as the critical care paramedic for their platoon," said Carpenter.
For commanders having a Soldier away from their unit training for two weeks is a significant amount of time. Yet ask any of the students that have gone through the course and each will agree it is a worthwhile investment. Aviation units benefit from having trained flight paramedics able to provide critical care beyond the basic 68W requirement. "We teach them a lot, but these skills are perishable. We emphasize that when students return back to their aviation units they need continuous training, the same as civilian flight paramedics," said Sergeant Carpenter.
"Our goal is to show Soldiers what it's like in the field. We want them to know what to expect, so they're prepared to save lives," said Major Capan. "The Army has an incredible battlefield injury survival rate. Yet there were a number of Soldiers we weren't able to save because they didn't receive critical care treatment in time. Now the Soldiers we're training in this course are equipped to save those lives. We're closing the gap with each flight paramedic we train."








Social Sharing