The labor and delivery unit of William Beaumont Army Medical Center, in conjunction with the chaplain's office, conducted a perinatal bereavement course at the hospital Oct. 16 to enhance care to grieving families when an infant dies.
This training is conducted many times throughout the year for the staff, and for the first time, a parent who experienced an infant death came forward to share her story in hope that attendees would gain a better understanding of what grieving families go through.
Jamie Walker, an Army veteran and now Army spouse, shared her experience when her daughter, Hali'a Rose Walker, was stillborn at 21 weeks gestation.
"There is no magical word or saying for moms and dads who go through this," Walker said. "Nothing you could say is going to make the pain go away. I remember people kept telling me they were sorry, but my anger would make me lash out at them."
While stationed in Hawaii, Walker went in for a routine check-up during her pregnancy in late September 2012. Her fundal height didn't check out to be normal and an ultrasound revealed her daughter had spina bifida. It was then that Walker felt angry, confused and frustrated, questioning why this was happening to her child.
Several weeks later, Walker came down with a fever and immediately went to the hospital. An ultrasound revealed Walker's daughter passed away and her body seemed to be reacting to the death as a toxin, hence the fever. Walker and her husband decided to induce labor right away and Hali'a was born Oct. 5, 2012 at 1:13 p.m. She weighed one pound, six ounces and measured 11.25 inches.
Walker described her emotions and feelings during the training. She also, in detail, described every staff member's action the day Hali'a was born.
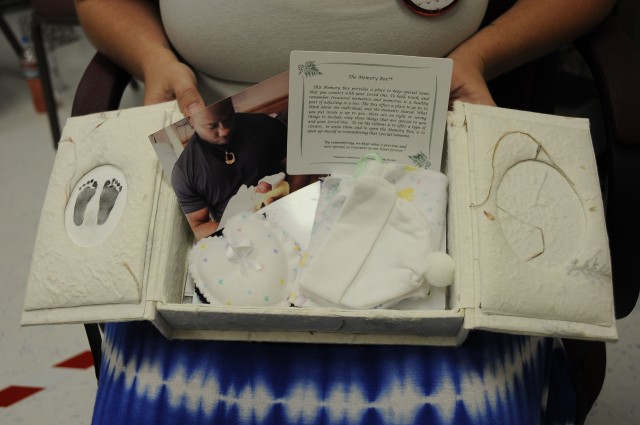
"We weren't prepared for this," Walker said. "We weren't prepared for anything, but the staff did take photos for us and printed them out and gave them to us. They gave us a memory box with the clothing she wore (after) she was born and they took her baby feet-prints to be included in the box. I really do appreciate what the staff did. I can tell you that I remember every single nurse's name in that room that day. That's how much detail I remember, so your words and actions will stick with the parents who go through this."
Walker told the attendees it took about a year and a half for her anger to subside. She found closure in the memory of the doctor's tears of sympathy.
"It showed to us that they really cared," Walker said. "The best you can all do is just have compassion."
The funeral for Hali'a was held a few days after her birth. Walker was thankful for the staff's compassion for her daughter. "All she knew was love," Walker said. "For the time she was here, all she knew was love."
Walker ended her story by answering questions from the nurses and sharing the pictures of her daughter hospital staff members gave her.
Maj. Kimberly Rosenbaum, clinical nurse specialist with the labor and delivery unit, WBAMC, along with Chaplain (Capt.) Troy Blan, scheduled the training and a mix of nurses from the unit and the mother-baby unit attended the training.
"Jamie's generosity in sharing her time and her openness about both the positive and negative aspects of her experience greatly enhanced the class," Rosenbaum said. "Many participants approached me and told me how much Jaime's story enhanced their understanding of the experience of living through a baby's death."
Walker plans to participate in the next bereavement training.
"I want the nurses to understand that they need to have compassion," Walker said. "Whether it's a miscarriage, a still birth, or an infant death, they all lost that 1-year-old they were going to have. They lost the 16-year-old they were going to raise. They lost the daughter they were going to walk down the aisle. Whether it was six weeks or 49 days after birth, they still all lost that. That's the biggest thing I want them to understand is that, we don't have the baby to breastfeed or hold, and we are going home to an empty house."
Rosenbaum plans to hold the next bereavement training session in December and will invite nurses and staff from other departments in the hospital, to include the emergency room, midwives and obstetricians.





Social Sharing