FORT DETRICK, Md. (July 8, 2014) -- A team of scientists scans the surface of severely burned skin, creates a three-dimensional map of the wound with a laser, and then prints skin cells onto the patient using a 3-D bioprinter.
Medical specialists are developing methods to transition this research from the laboratory to clinical trials.
The U.S. Army is a significant proponent and investor in regenerative medicine and 3-D bioprinting, according to officials. Scientists are aiming to advance this new research area to help injured service members recover from the wounds of war.
Dr. Michael Romanko, who provides science and technology management support for the Tissue Injury and Regenerative Medicine Project Management Office, or TIRM PMO, with the U.S. Army Medical Material Development Activity, said that improvements in body armor, vehicle design and advanced medical care during the past decade led to Soldiers suffering injuries that would have caused fatalities in previous conflicts.
Blasts from improvised explosive devices have increased the number of Soldiers experiencing the loss of limbs, catastrophic injuries to the face and severe burns.
"There was an increasing need to deliver therapies for wounded warriors. We saw a spike in the severity of the trauma that these Soldiers were receiving. As we increased the quality of battle armor, the injuries they were surviving were that much more debilitating," said Romanko, who holds a doctorate in molecular medicine.
The Department of Defense, in turn, established the Armed Forces Institute of Regenerative Medicine, or AFIRM, in 2008. Regenerative medicine aims to replace or regenerate human cells, tissues or organs to restore or establish normal function.
The AFIRM is a multi-institutional, interdisciplinary network of universities, military laboratories and investigators under the framework of a cooperative agreement, Romanko said. The network is designed to promote integration of development, from basic science research through translational and clinical research, as the best means of bringing regenerative medicine therapies to practice.
The success of the first five years of the AFIRM led to the competition of a new cooperative agreement in 2013, he said.
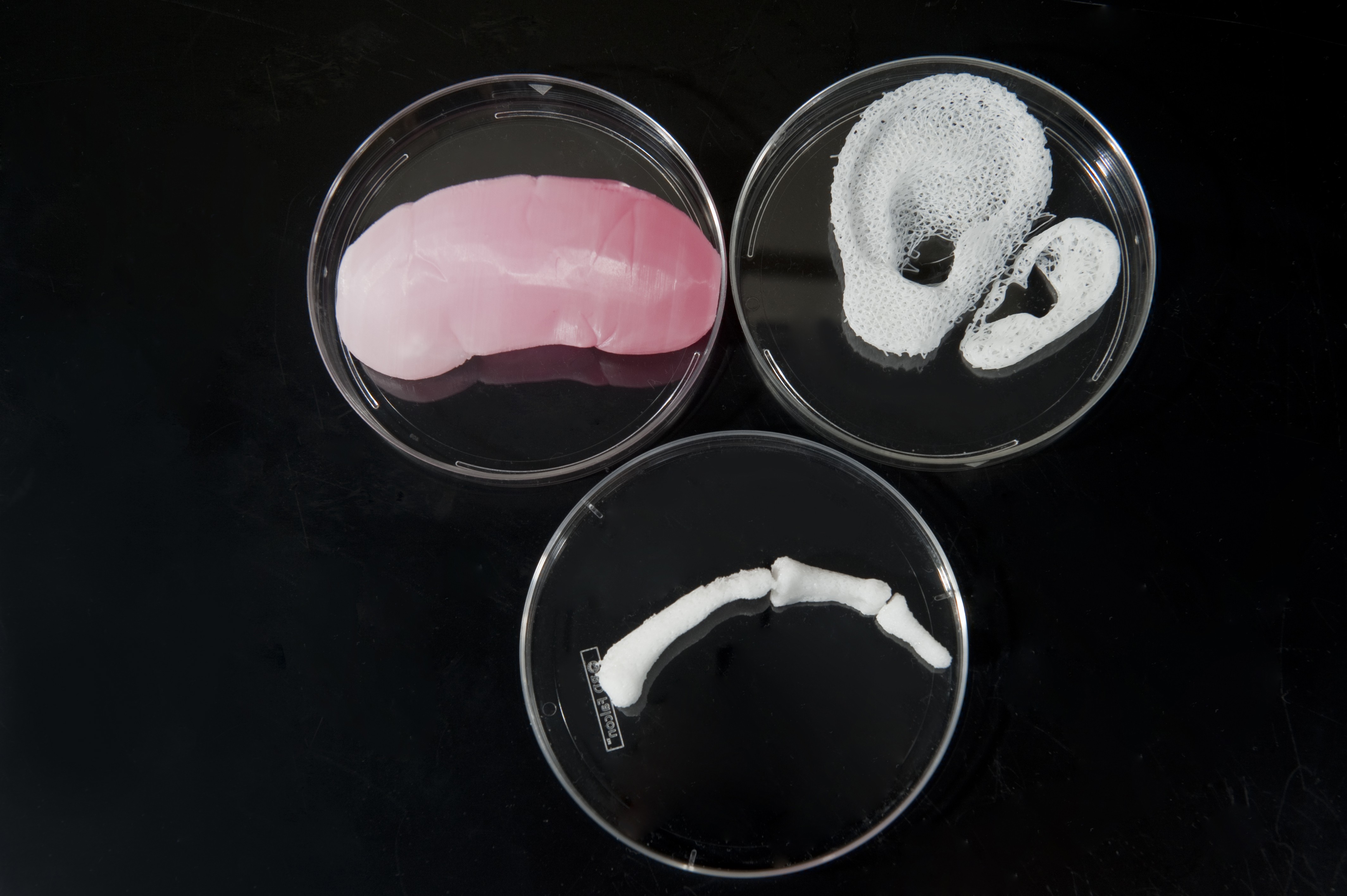
3-D bioprinting is one tool that scientists are developing in the field of regenerative medicine. It is an early discovery technology being used to address extremity injury and skin, genitourinary and facial repair by AFIRM investigators.
Skin repair is the most robust focus area addressed in the regenerative medicine portfolio, Romanko said.
"The scars that Soldiers develop as a result of burns constrict movement and disfigure them permanently. The initiative to restore high-quality skin that is elastic and complete with sweat glands, appropriate pigmentation and hair follicles is incredibly important," he said.
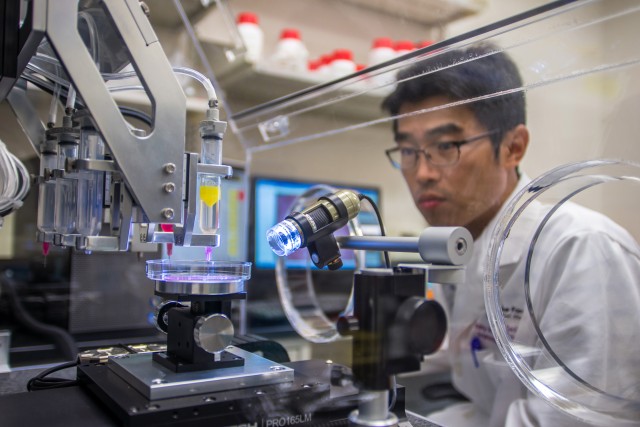
Romanko described how researchers are currently using 3-D bioprinters for skin repair research.
In translating this technology to the clinic, scientists will take healthy cells and, using a device similar to an inkjet printer, load the cartridges with two types of skin cells -- fibroblasts and keratinocytes -- instead of ink. Fibroblasts make up the deep layer of skin, and keratinocytes compose the top layer.
After the team completes a scan of the burn and constructs a 3-D map of the injury, the computer tells the printer where to start printing and what type of cells to use, depending on the depth of the injury and the layer being reconstructed. The bioprinter deposits each cell precisely where it needs to go, and the cells grow to become new skin.
Early research results are promising, and scientists hope this could be a viable solution in the future, Romanko said.
Addressing the need for skin repair is important, because burns account for 10 percent to 30 percent of battlefield casualties. The precision available through 3-D bioprinting allows for a custom solution for each patient.
"Everyone has a different type of injury, and not everyone's skin injury looks the same. Skin bioprinting would provide a scalable form of personalized medicine," Romanko said.
An additional goal in regenerative medicine is bioprinting organs, limbs and vascular systems. Other early discovery 3-D bioprinting projects within AFIRM have focused on the generation of complex tissue components with bone and muscle.
3-D bioprinting is still in the early stages, Romanko said. More laboratory research is necessary, and several federal regulatory steps must be completed before patients could enroll in clinical trials.
About 30 universities, hospitals and additional partners, led by the Wake Forest Institute for Regenerative Medicine, make up the consortium of AFIRM researchers. Romanko works with the TIRM PMO, which supports AFIRM and other regenerative medicine programs.
AFIRM receives funding from the U.S. Army, the Office of Naval Research, Air Force Surgeon General's Office, Veterans Health Administration, National Institutes of Health and the Office of Assistant Secretary of Defense for Health Affairs. AFIRM investigators also bring in funding from other federal, state and private sources.
Leveraging experts from across academic and medical research organizations allows the Army to pull together the range of specialties needed for this type of complex technology, Romanko said.
Engineers work with bioimaging experts to develop the actual bioprinters and technology to scan the topology of injury sites, like the skin, or recreate the 3-D structures of other organs. In turn, biologists and physicians who specialize in the specific organ or tissue being produced oversee the process to ensure the appropriate placement of cells and construction of tissue. They all work together as a multidisciplinary team to advance bioprinting research.
Expanding the technology to a greater number of potential patients will also help to ensure its long-term viability, Romanko said.
"This has very widespread use, not only to the military audience, but also to the civilian population. We need a larger commercialization audience in order to be a self-sustaining technology," he said.
Related Documents:
Army Technology Magazine (PDF) [PDF]



Social Sharing