WASHINGTON (Army News Service, June 14, 2007) - Medical Engineer Technician Carlos Villamizar uses a dental pick to scratch between the crevices of a hard plastic model.
He picks and picks and picks, scraping away unwanted milky-yellow plastic material, bringing the model to a near-perfect replica of the male patient's lumbar spine it represents.
Mr. Villamizar then blasts it with pressurized air -- and continues picking some more. It's tedious and time consuming, but every minute he spends on the model translates to less time the patient has to spend in the operating room.
From the time the surgeon makes the first cut in the operating room, every minute counts for the patient.
The longer the wound is open, the greater the chance of infection and the more blood is lost. The longer the patient is under anesthesia, the greater the risk of respiratory issues.
Walter Reed Army Medical Center's 3-D Medical Applications Center uses technology originally designed for the manufacturing industry to cut down on the amount of time a patient is in surgery by as much as six hours.
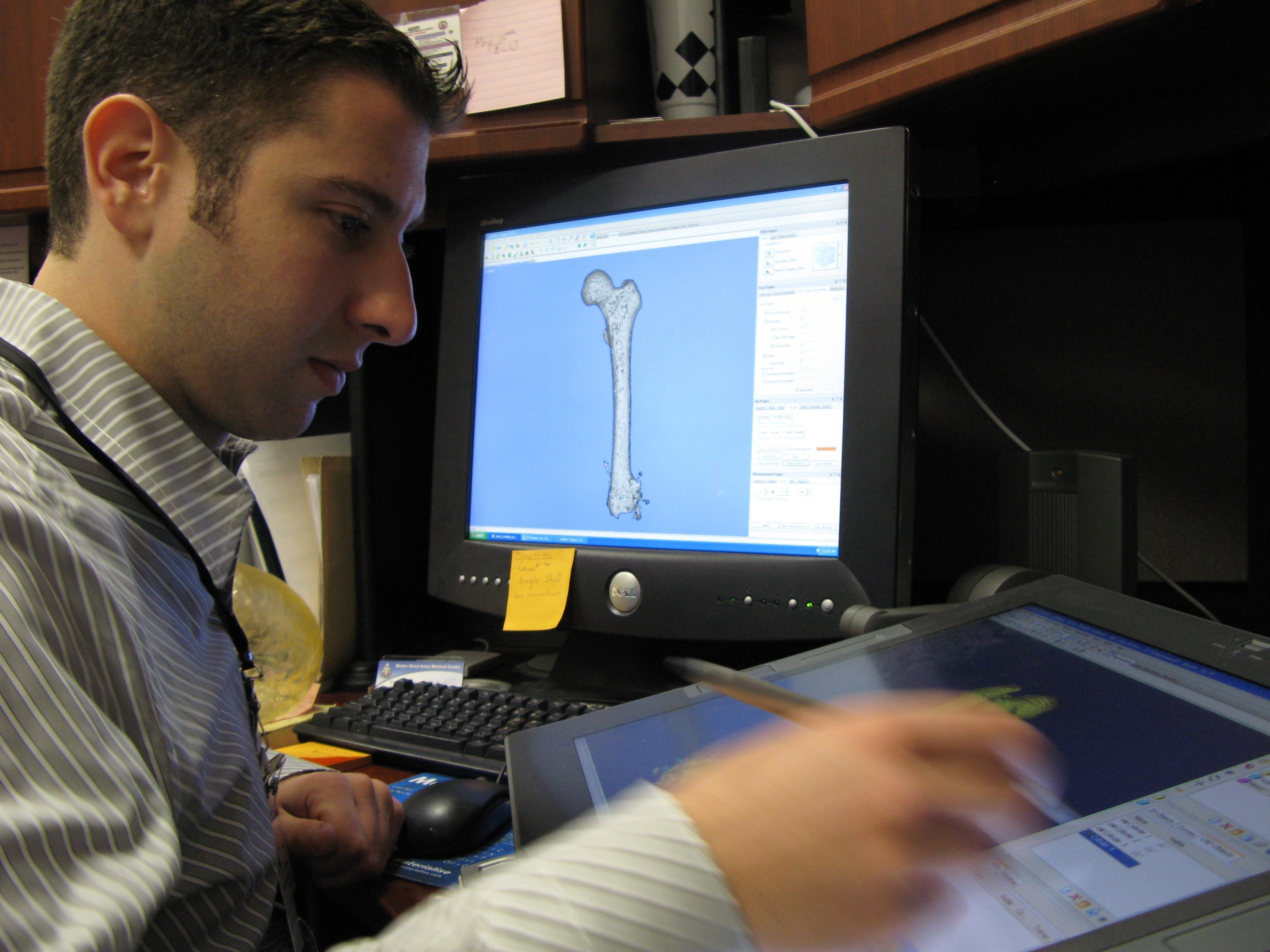
The one-of-a-kind lab in military medicine creates hard-plastic, 3-D "medical models," or replicas, of injured body parts based on CT scans. So instead of a surgeon looking at a series of transparent scans in preparation for surgery, they have a replica of the injured bone or skull that they can literally hold in their hands and examine.
This helps them not only determine the best approach to surgery, but also allows them to fabricate and fit implants prior to the surgery.
"You have visualization outside the body. You don't have to peel back all of the tissue and all of the muscles to get the same level of visualization," said Dr. Stephen Rouse, a retired military dentist who runs the lab with a staff of two.
"You are giving the surgeon and his team, and the patient, an opportunity to see exactly the same thing, to be able to determine where and how they are going to operate. The patent can make a much more informed decision," Dr. Rouse said.
In many cases, having a model prior to the surgery reduces the size of the incision the surgeon must make, and ensures greater accuracy in the operating room, Dr. Rouse said. CT scans provide a general picture of the surgical area, but the 3-D medical model allows surgeons to see and touch beforehand what they will eventually see and touch in the operating room.
This gives surgeons a critical advantage when dealing with the current medical phenomenon of heterotopic ossification, or HO, occurring frequently in Iraq war amputees. HO is new bone growth in abnormal areas. Doctors are puzzled as to why it is occurring in so many amputees from the war.
The growth is random and can form a lacy network of new bone under the skin, similar in appearance to coral formations.
The growth can cause serious problems for the amputees, especially when fitting and wearing prosthetics. The bone can grow and rub and make wearing a prosthetic unbearable. Often additional surgeries are needed to remove the HO, but it sometimes encapsulates major arteries or nerves, making the surgery risky.
The medical models show three-dimensionally the HO formation and where it is attached. It can also highlight any major arteries in the area. Surgeons look at the models to decide at which point they want to enter and which cuts will yield the best results, Dr. Rouse said.
"(With CT scans,) what you cannot see is a full definition of 'Where is this' Where is it fastened to the pelvis' What anatomic objects do I have to watch out for if I'm going to remove it'" Dr. Rouse said.
"The surgeon is going to look at (the medical model) and find the areas where they are going to gain the most by removing it," he said.
The technology behind the model making first was developed for the manufacturing industry for quickly building prototypes. It is used on several military installations for prototyping parts prior to manufacturing, Dr. Rouse said. It also is used in aviation and car manufacturing.
The largest single owner of the SLA 7000, or stereo lithography apparatus, used at Walter Reed, is Align Technology, Inc., the makers of the Invisalign invisible braces, Dr. Rouse said. They own 40 of the machines, he said.
It was first introduced to military medicine in the early 90s by Dr. David Chance and Dr. Stephen Schmitt, both Air Force dentists looking for a way to speed up the process of making bridges and partial dentures, Dr. Rouse said. It was first used in an Air Force dental clinic at Wilford Hall Medical Center, at Lackland Air Force Base, Texas. Since its inception in medicine during the early 90s, stereolithography has had limited use, primarily in orthodontics and oral and maxillofacial surgery, Dr. Rouse said.
The technology also is used when planning to separate conjoined twins, looking at tumors in bones, deciding treatment for aneurisms, and examining malformations in the brain, Dr. Rouse said.
Walter Reed is the only military hospital to operate a full medical service bureau and makes its services available worldwide to anyone in military medicine, Dr. Rouse said.
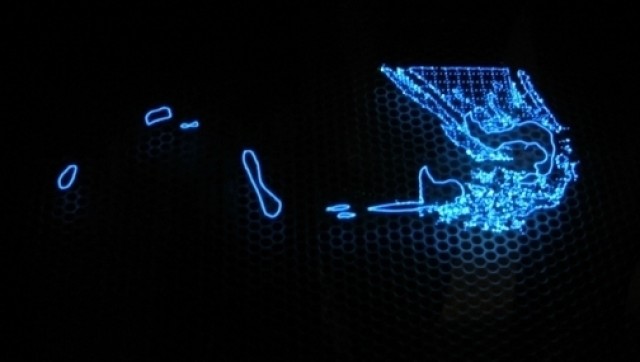
The 3-D medical model-making process starts with the CT scans of the injured area. A computer program interprets the electronic CT scan data and renders a 3-D computer image. The image is cleared of extraneous data and then sent to the SLA 7000.
The SLA 7000 is filled with a vat of liquid resin. A perforated platform in the vat slowly drops one-tenth of a millimeter at a time, as a laser dances across the surface and "prints" each layer. The layers bond the laser activates the resin.
The vat holds about 320 kilograms of resin, costing about $200 per kilogram, or a total of $64,000. A model of a pelvis uses about $500 worth of resin. The model saves thousands of dollars in operating room expenses, Dr. Rouse said, because of the timesavings. Dr. Rouse said he has documented a savings of two to six hours per surgery in which the models were used.
"The cost of the model is a miniscule part of the equation," Dr. Rouse said.
The process of printing the model is called a "build." Multiple models are built simultaneously. A model of a full skull including the jaw can take about 18 hours. Larger, more complex builds can take more than 50 hours to finish, Dr. Rouse said.
Once built, the model is rinsed, cleaned and cured. That takes a couple of hours, Dr. Rouse said. The lab can process, build and ship a model typically within 72 hours.
Since opening in 2004, the lab has created more than 1,600 models for about 580 patients, Dr. Rouse said. Some patients require multiple models so the surgeons can track the healing progress, he said.
(Fred W. Baker III writes for the American Forces Press Service.)




Social Sharing