Editor's note: This is the second in a three-part series of articles designed to generate awareness and provide resources for people suffering from seasonal affective disorder and depression.
America's involvement in conflict overseas has changed a lot of things-from budget battles on Capitol Hill to an increase in combat veterans serving. It has also evolved matters surrounding behavioral health, including a decrease in negativity with regard to service members seeking behavioral health help.
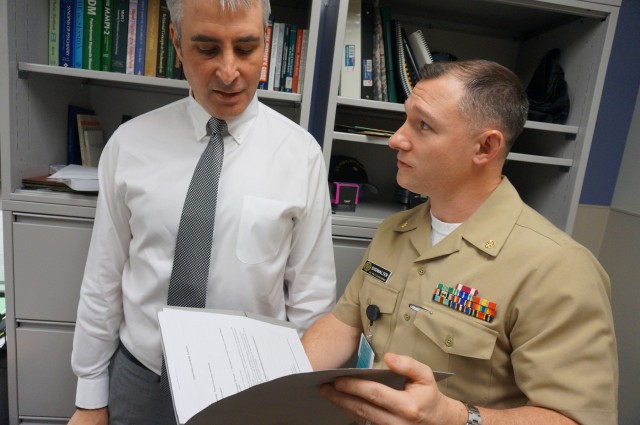
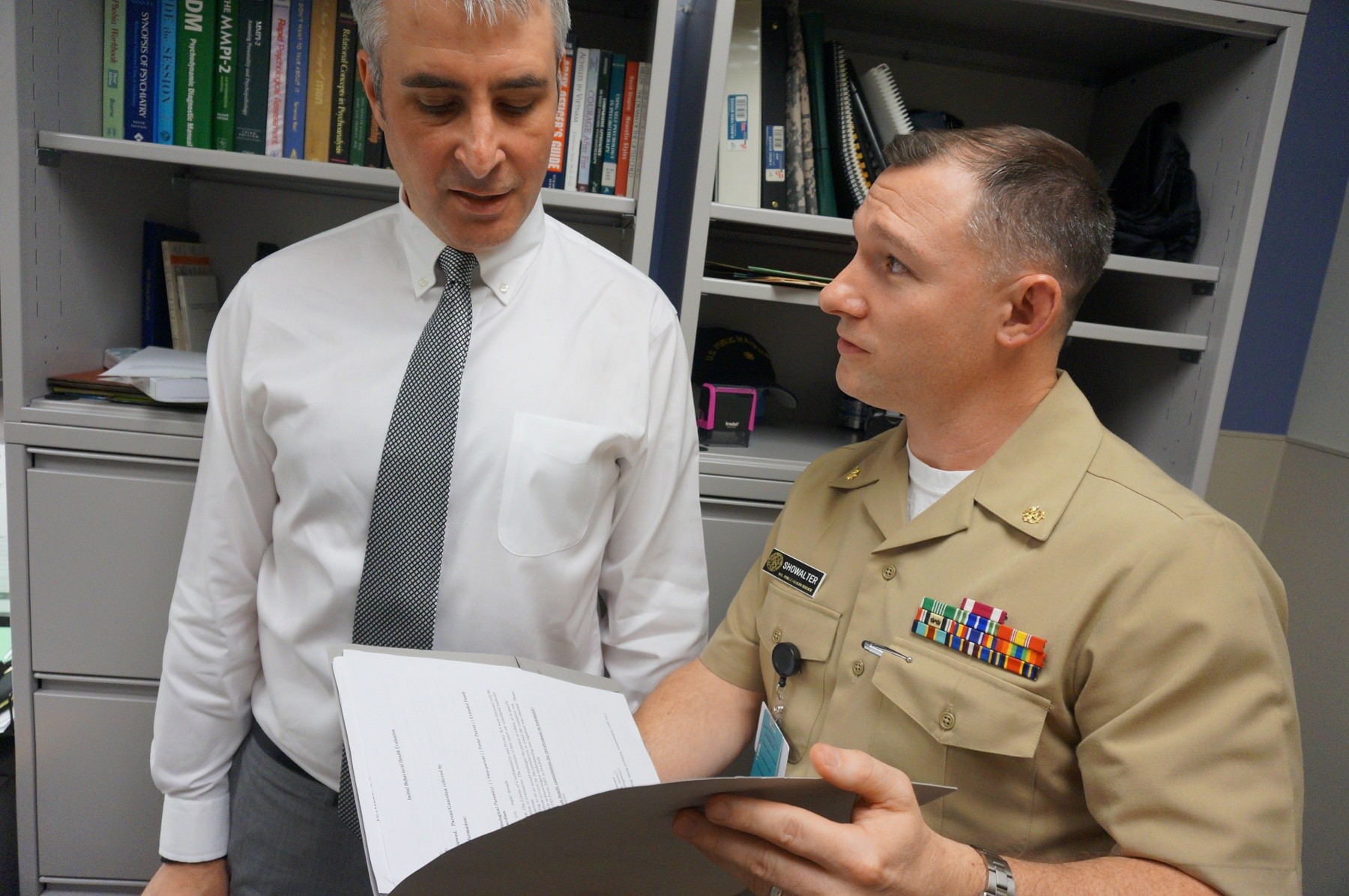
"That's the change I've seen that's outstanding," said U.S. Public Health Service Lt. Cmdr. Jeff Showalter, chief of Behavioral Health at Andrew Rader U.S. Army Health Clinic. "Leaders are coming [to Behavioral Health] themselves, many of whom had two, three or four deployments who come in at the urging of their partner."
Factors like this highlight the collaboration and communication between service providers, including medical professionals and religious support personnel, to provide help to those who seek it. At Joint Base Myer-Henderson Hall, Andrew Rader U.S. Army Health Clinic's Behavioral Health staff and joint base chaplains have seen a spike in service members seeking help. But each resource has a different responsibility helping people cope.
"It's not our job to diagnose depression: we don't have the medical insignia on our collar, we have a cross on our collar," said U.S. Navy Lt. Chad Goddard, chaplain for Headquarters and Service Battalion on the Henderson Hall portion of JBM-HH. "But we can still identify the signs of depression when we see them. I'll say 'Let's go talk to a behavioral health doctor about this or a family health counselor.' Chaplains are a very good clearing house."
Depression, seasonal affective disorder and adjustment disorder 101
Particularly, during the winter months service members could be facing depression, or variants of seasonal affective disorder and adjustment disorder, Showalter explained. Life altering changes like a new duty location, a new financial hurdle, or a major relational issue are examples of times of transition that are significant contributors for depression and stress, he said.
"This is the time [of year] we see perhaps an elevation in the number of referrals," Showalter said. "The hallmark of a major depressive episode is that an individual experiences depressed mood, most of the day, nearly every day."
Still, referrals to behavioral health do vary throughout the year, but the winter holidays "could be a variable in seeking help," explained Showalter.
Further, Showalter defined additional hallmarks of a major depressive episode as when an individual experiences "diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day; weight loss or gain (of at least 5 percent) in a month; insomnia or hypersomnia; fatigue or loss of energy nearly every day; feelings of worthlessness or excessive guilt; diminished ability to think or concentrate and/or recurrent thoughts of death / suicidal ideation.
"These symptoms must be continuous for the span of [two weeks] to meet diagnostic criteria for a Major Depressive Disorder," said Showalter. "While financial and personal stressors could potentially progress toward clinical depression, they are more often transient and resolve without the need for behavioral health intervention."
Showalter said that service members who suffer from depression, or variants of depression, will then experience "a loss in pleasure and activities; they're isolating more; hypersomnia, insomnia, increased weight and depressed mood."
A recurrent depression is best treated with medication and therapy, said Showalter.
In the event that treatment was unsuccessful in restoring a service member to being fit for full duty to include deployment, then referral to the Medical Evaluation Board would be warranted.
The Behavioral Health Service at Rader Clinic is staffed by three psychologists, two social workers, and a psychiatrist ready to assist with symptoms of depression or another psychiatric condition.
Currently, only active duty personnel are eligible for behavioral health services, according to Showalter.
"We see any and all people who are assigned [to Joint Base Myer-Henderson Hall regardless of rank]," he said.
Informed consent and confidentiality within Behavioral Health
Service members are immediately advised of the confidentiality agreement associated with seeking help within Behavioral Health, according to Showalter. This is the first conversation the service member will have with a Behavioral Health rep, before discussing matters related to what originally brought them to Behavioral Health. Service members are also advised of the type of matters that would require confidentiality to be broken.
"There are only a few instances where information would go back to their [the patient's] command," Showalter said. "For instance, if the service member said they were going to kill themselves or somebody else or that a child or elderly person was being abused-in those instances, absolutely I'm going to have to break their confidentiality to protect those other people-or to protect them [the service member]."
But there are other circumstances which could result in a break in confidentiality to include a person who is a danger to him or herself, or someone who may be psychotic.
Only in these circumstances is confidentiality broken, he said. Still, Showalter advises people with an aversion to seeking treatment at Behavioral Health to metaphorically liken it to a physical injury left untreated.
"It is likely to worsen," Showalter said. "The condition could become worse than it was. Some conditions don't go away on their own...We want to talk with people about what might be helpful, what has proven helpful in the past, so we can put together the best treatment plan possible," Showalter said.
Service members who want support from Behavioral Health at Andrew Rader U.S. Army Health Clinic should call 703-696-3456. Counseling, therapy and medication treatments are offered.
Upon entry, service members complete an "intake process" to determine individual treatment needs. They are later paired with specialty providers who best suit those behavioral health needs, according to Showalter.
Additionally, Marine and Family Programs at Henderson Hall provides a wide variety of counseling services within its Community Counseling Program (CCP). Call 703-614-7204 to learn more.
Social Sharing